Physicians and other medical practitioners may very well verify that one of the most common sleep disorders of modern age is Narcolepsy, which seems to be affecting more and more people all around the world due to demanding lifestyles and economic reasons.

( Narcolepsy – Image Courtesy of www.empowher.com )
Classification of Types of Narcolepsy
The ICSD-2 (International Classification of Sleep Disorders, edition 2) is an internationally approved, medical standardization recognized and utilized by medical professionals as a glossary outlining and categorizing all the known sleeping disorders. It clearly stipulates various types of Narcolepsy which is categorized into 3 related yet distinct classes as follows:
1. Narcolepsy without Cataplexy
2. Narcolepsy with Cataplexy (also known as Narcolepsy Cataplexy Syndrome)
3. Secondary Narcolepsy
Thereby the main focus here is on the type of Narcolepsy that is incident without Cataplexy, which is rather distinct from the Narcolepsy Cataplexy Syndrome.
( ICSD-2 – Image Courtesy of durmiendomejor.com )
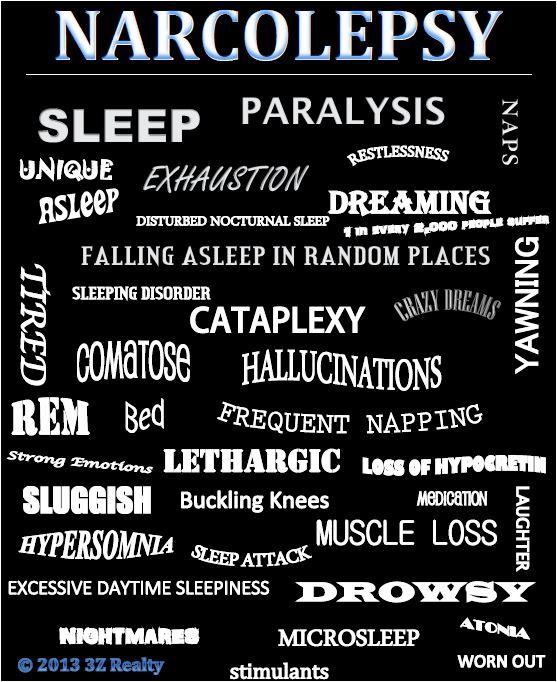
What are the symptoms of Narcolepsy?
Clinical manifestations of Narcolepsy are shown to commonly reach peak levels in patients between the age bracket of 15 years to 30 years old.
Some of the most common complaints made by people suffering from Narcolepsy include: EDS (Excessive Daytime Somnolence or Sleepiness), intense desire and constant urge to go to sleep, as well as feeling rather refreshed and rested after catching extra sleep during the day (in addition to already having slept during the night, but not refreshed by nighttime sleep by the time one wakes up in the morning).

( Narcolepsy – Image Courtesy of blog.mattressesforless.net )
However, the above complaints are also closely linked to other sleeping disorders, and therefore further investigation and analysis is necessary on the part of the medical practitioner lest a misdiagnosis is made; for instance, as Partial Arousal Disorder, Insomnia, or Obstructive Sleep Apnea Syndrome (OSAS).
It is critical that a proper investigation be conducted on the part of the medical practitioner because if misdiagnosis occurs and the medicines prescribed by the doctor on the basis of wrongful diagnosis negatively affect a patient’s health, it may land him in something extreme. For example, the patient can file a medical malpractice lawsuit against him by hiring a lawyer from a law firm (read more here about the law firm that deals with medical negligence). As a result, doctors may need to pay more attention to diagnosis rather than lumping all problems together.
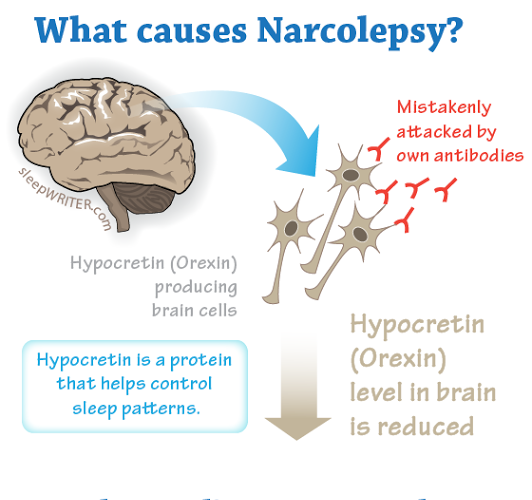
( Narcolepsy Cause – Hypocretin or Orexin – Image Courtesy of healthresearchfunding.org )
Major Narcolepsy Symptoms with Figures of Occurrence
- Sleep Attacks (of the Narcoleptic nature) – 100 per cent prevalence
- Sleep Paralysis – 25 to 50 per cent prevalence
- Hallucinations (Hypnagogic in nature) – 20 to 40 per cent prevalence
- Cataplexy – 60 to 70 per cent prevalence
- Automatic behaviour – 20 to 40 per cent prevalence
- Impaired nighttime sleep – 70 to 80 per cent prevalence

( Narcolepsy and Falling Down – Image Courtesy of www.itv.com )
Co-morbidity or concurrent or secondary occurrence of Narcolepsy with other sleeping disorders cannot be ruled out or ignored. In many cases of patients diagnosed with Narcolepsy, an additional co-morbid diagnosis of one of the following sleep disorders is also observed:
- PLMS – Periodic Limb Movements in Sleep
- Sleep Apnea
- Nocturnal Eating Disorder
- RBD – REM (Rapid Eye Movement) Behavior Disorder
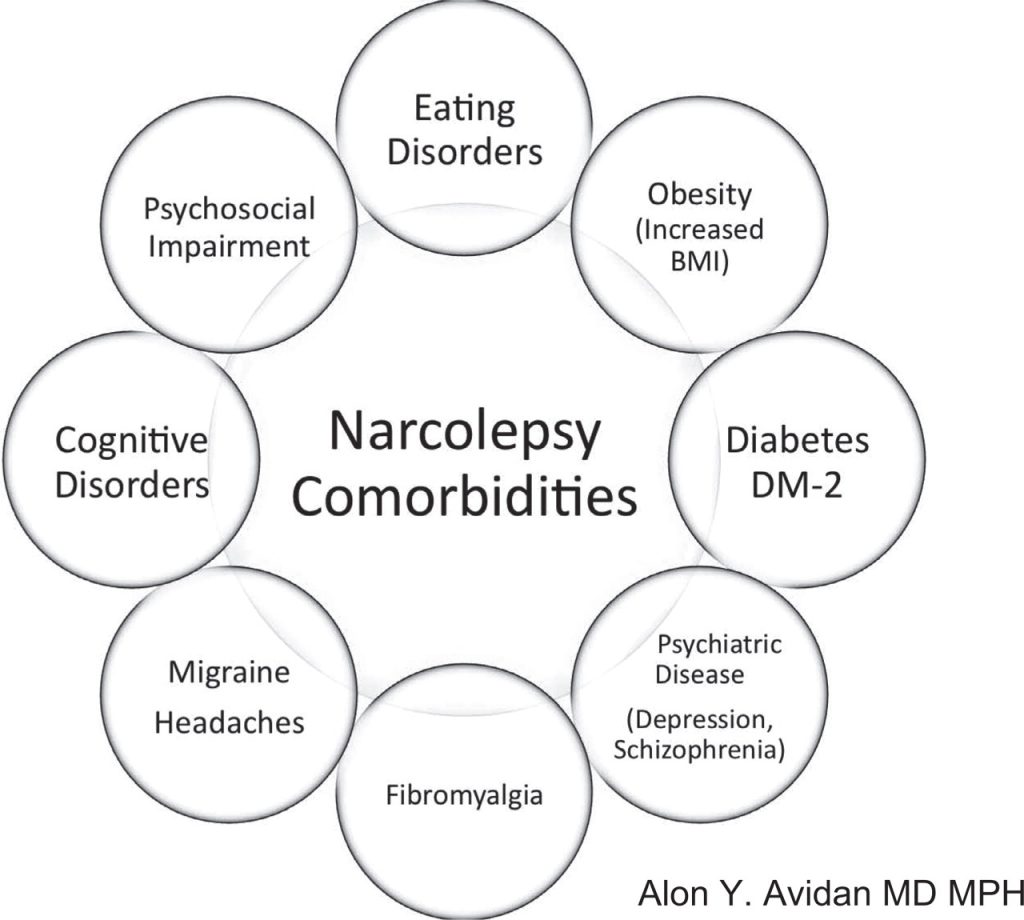
( Narcolepsy Comorbidities – Image Courtesy of books.publications.chestnet.org )
Various sleep disorders are genetic as they may be passed on, and Narcolepsy is one among these; therefore gathering patient data on the family background is necessary for the diagnosis of Narcolepsy. Fortunately, with the developments in healthcare data analytics and AI in general, medical professionals can easily acquire comprehensive information related to a patient’s healthcare journey.
( Narcolepsy Symptoms – Image Courtesy of www.pinterest.com )
Differentiating between Narcolepsy and Hypersomnia
It is also possible for a case of Narcolepsy to be misdiagnosed as Hypersomnia (specifically primary or idiopathic Hypersomnia) to which it is very closely related – they both have the same age bracket of disorder onset, but the sleeping patterns observed in Narcolepsy differ from those associated with idiopathic Hypersomnia.
One of the key differences is that while additional daytime sleep or napping is observed to be refreshing and restorative in Narcolepsy, the same is not the case with Hypersomnia, whereby the patient sleeps for long extended durations of sleep that is non-refreshing and non-restorative, thereby constantly desiring to fall asleep while the Narcoleptic patient is usually well rested after catching some extra sleep during the day.
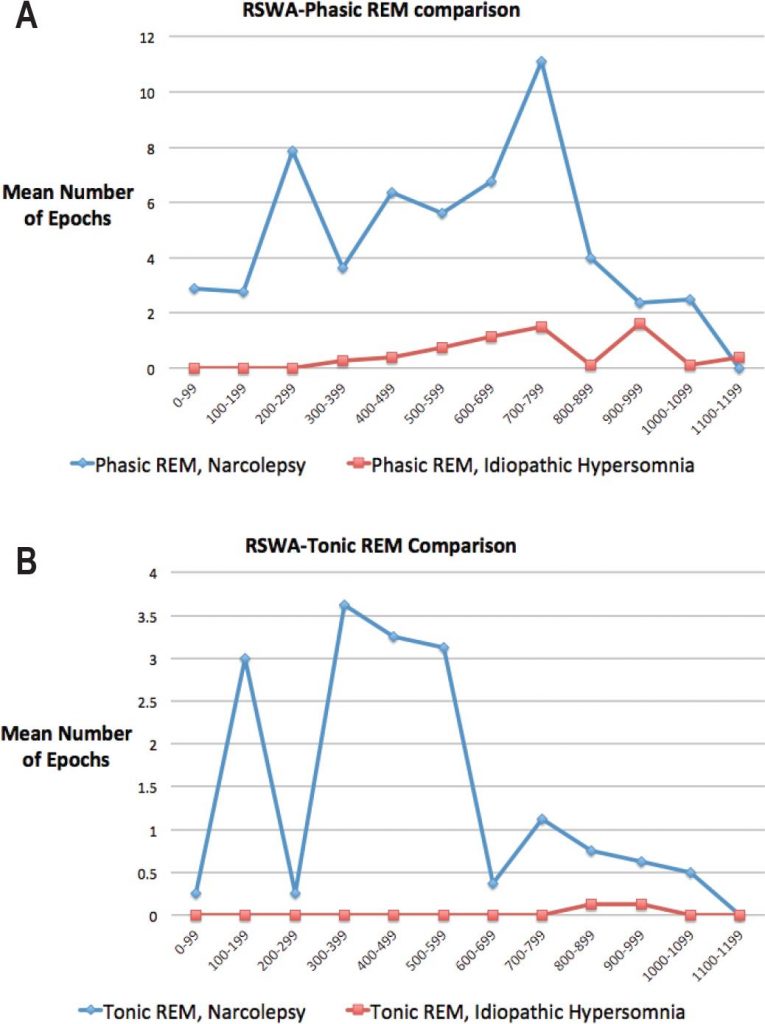
( Narcolepsy vs. Hypersomnia – Image Courtesy of www.aasmnet.org )
Differentiating between Narcolepsy and Sleep Apnea
An underlying case of Narcolepsy may also be misinterpreted as a case Sleep Apnea, particularly due to the EDS (Excessive Daytime Somnolence) or Daytime Sleepiness presented in both Narcolepsy and Sleep Apnea.
In this case, a clear distinction should be made with other symptomatic manifestations of Sleep Apnea not presented in Narcolepsy, such as: snoring, frequent and constant awakening from one’s sleep all through the night, cataplexy and cessation of breathing; all of which are typical symptoms of Sleep Apnea, specifically Obstructive Sleep Apnea Syndrome (OSAS), and are not typical of Narcolepsy.
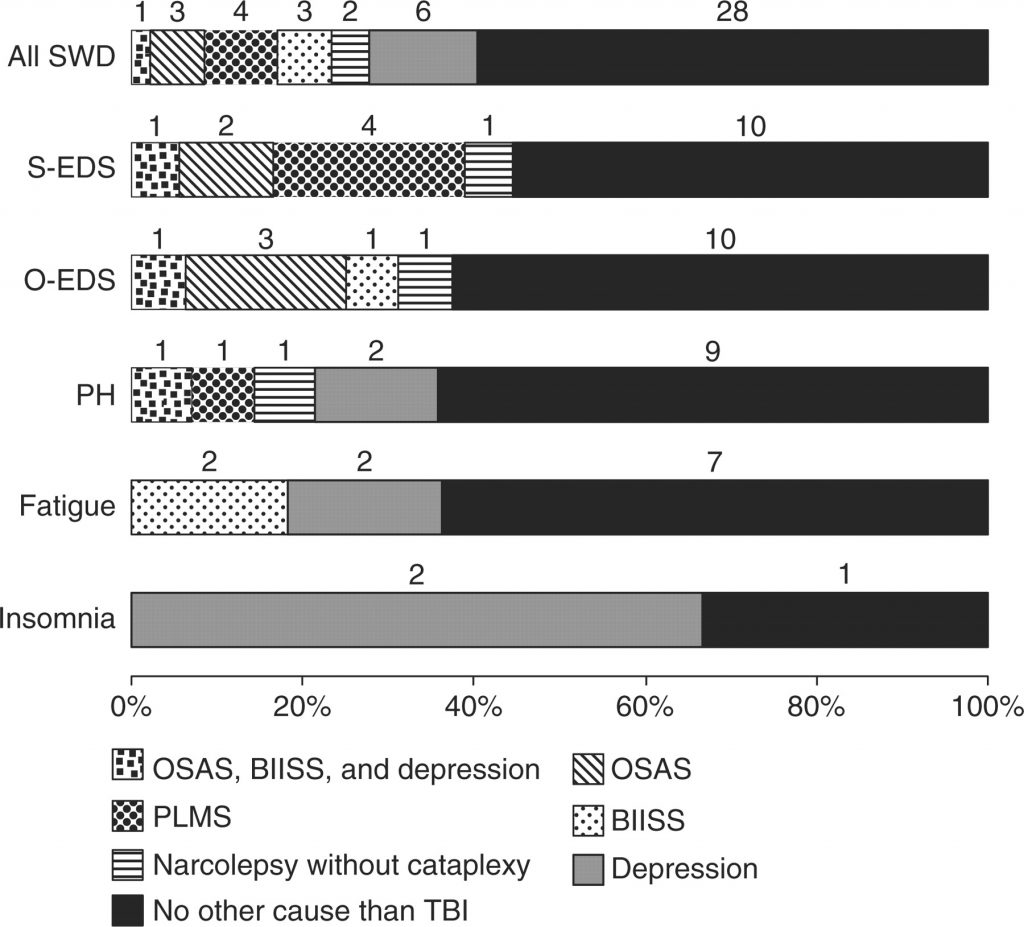
( Sleep-Wake Disturbances in Sleep Disorders Comparison – Image Courtesy of brain.oxfordjournals.org )
Lab Analysis and Testing for Narcolepsy
The Polysomnograph – PSG Test, used to diagnose Obstructive Sleep Apnea Syndrome (OSAS), may be run overnight to assess the sleep disordered patient suspected to have Narcolepsy as it has been shown to also be beneficial in diagnosing Narcolepsy. With the PSG testing, various physiological factors are assessed, including the determination of optimized pressure measurements for CPAP – Continuous Positive Airway Pressure.

( CPAP Titration in OSAS Treatment – Image Courtesy of www.alamy.com )
MSLT – Multiple Sleep Latency Testing has been fundamental in the documentation, observation and analysis of pathological chronic sleepiness, such as that presented in patient cases of Narcolepsy. It quickly picks up on the latency of sleep onset that is detected to having occurred quickly in 8 minutes or less which is a key indicator for a Narcolepsy diagnosis. Another relative indicator picked up on by the MSLT in diagnosing Narcolepsy is the occurrence of 2 sleep onset Rapid Eye Movement (REM) phases obtained from the analysis of 4 to 5 sleeping or napping sessions.
( MSLT Multiple Sleep Latency Test – Image Courtesy of www.medscape.com )
On the other hand, an MWT – Maintenance of Wakefulness Test (which is a variation of the MSLT), may be beneficial in confirming a suspected case of Narcolepsy. However, it should be noted that Multiple Sleep Latency Testing is more superior to Maintenance of Wakefulness Testing which is less sensitive in detecting and diagnosing Narcolepsy. Nonetheless, the MWT is considered to be a more effective option in analyzing the effectiveness of treatment administered for Narcolepsy and other sleeping disorders like Obstructive Sleep Apnea Syndrome (OSAS) when being treated with CPAP Titration.
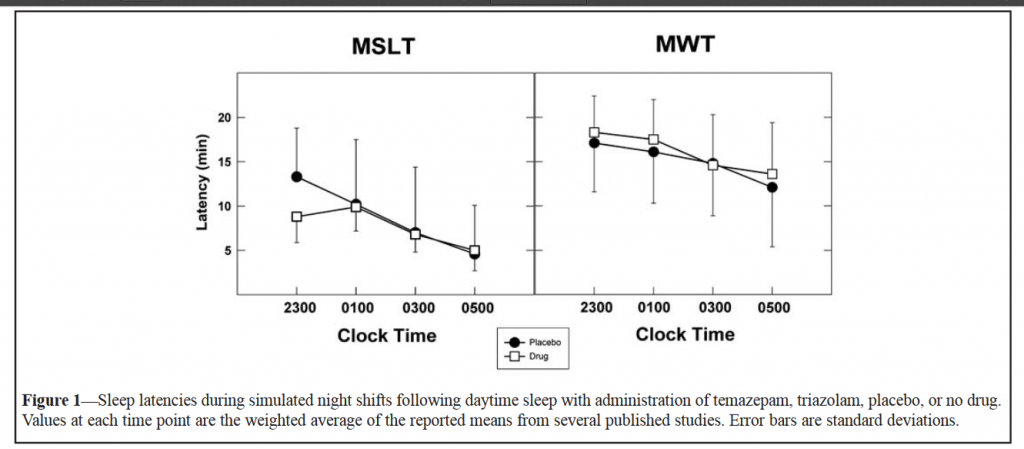
( MSLT and MWT – Image Courtesy of www.aasmnet.org )
Further, sleep experts have previously authored the possibility of mediation of Narcolepsy, among other sleeping disorders, by the leukocyte proteins called cytokines, in particular, IL-6 (Inter-Leukin) and TNF-α (Tumor Necrosis Factor).
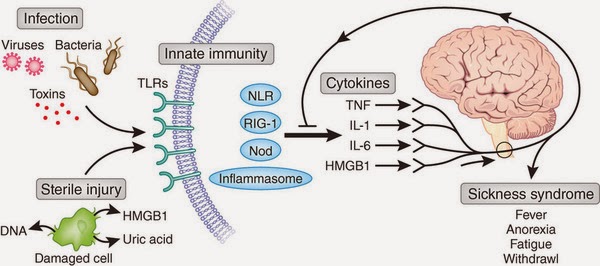
( Cytokines in Disease – Image Courtesy of biologicalexceptions.blogspot.com )
Thus histo-compatibility analysis of leukocyte antigens is also beneficial in diagnosing suspected underlying Narcolepsy in patients with a sleeping disorder.
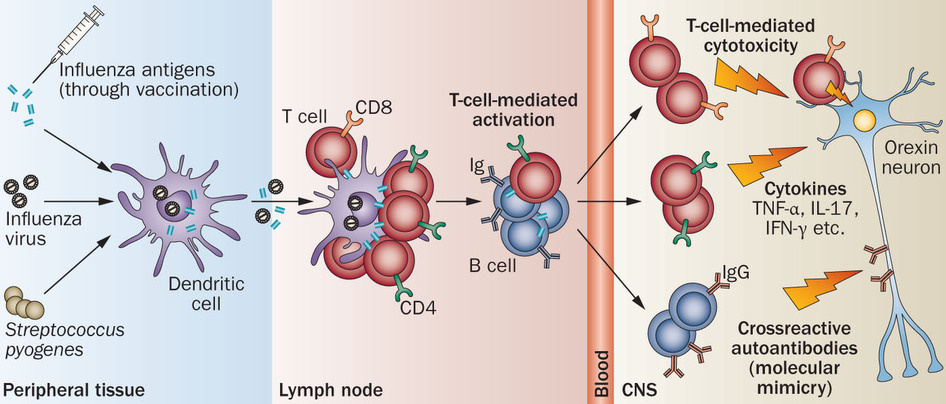
( Autoimmunity in Narcolepsy – Image Courtesy of www.nature.com )
In addition, analyzing fluid levels of Hypocretin-1, a cerebrospinal sample, may also confirm the diagnosis of possible underlying Narcolepsy in the patient.
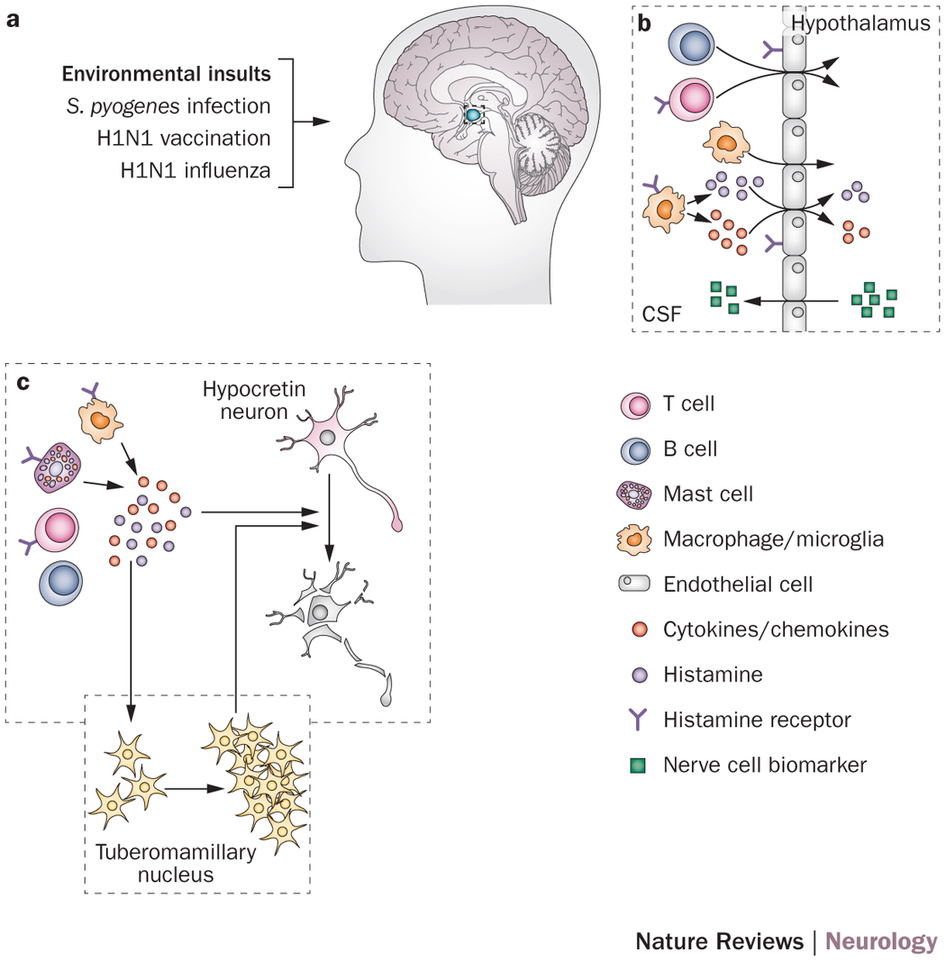
( Hypocretin from Hypothalamus in Narcolepsy – Image Courtesy of www.nature.com )
Sleep experts suggest the possibility of Narcolepsy actually being a degenerative medical condition that affects the neurons which contain Hypocretin within the lateral region of the hypothalamus.

( Narcolepsy – Image Courtesy of new.lakeforest.edu )

