Insomnia, perhaps the most rampant sleep disorder, so prevalent is it that some don’t even know they have it, or that what they experience has a name, or that it is an anomalous sleeping condition…!
( Insomnia – Image Courtesy of sleepingresources.com )
Symptoms of Insomnia
As a basic intro, Insomnia is one of the 4 most common sleeping disorders, and it symptomatically presents itself in one or all of these complaints:
- Having difficulty falling asleep (sleep onset)
- Having difficulty staying asleep (sleep maintenance)
- Constantly or frequently waking up in the middle of the night
- Waking up too early in the morning (premature awakening)
- Experiencing fatigue and exhaustion during the day (despite having slept at night)
- Low quality sleep that is not restorative, and not restful
- Aching, sore painful muscles
- Depression
- Moodiness and irritability
- Anxiety
- Poor or no concentration

( Insomnia – Image Courtesy of menhealthcare.net )
Analyzing Possible Insomnia
In a majority of patients, Insomnia remains a stubbornly persistent problem that affects their normal functionality and productivity during the day. The symptoms present themselves at least 3 to 4 times a week and prevail for extended periods of time, longer than 1 month while disrupting diurnal productivity and functionality. That is why many who are affected by this sleeping disorder often consider consulting a medical professional who can provide them with the right kind of medication to cure the ailment. However, there are some who often take the alternative route to medicines–cannabis products like Justin Trudeau Kush, which is known to instantly offer help.
( Insomnia – Image Courtesy of www.sleepeducation.org )
That said, the occurrence of Insomnia may be independent as a primary condition that is not necessarily caused by any other condition, or co-morbid occurring alongside another medical condition such as: neurological conditions, psychiatric disorders, cases of alcoholism, drugs and substance abuse. When the patient is affected by a case of acute Insomnia it is usually linked to a predominant stressful incident or event affecting the patient and disrupting their overall well-being and functioning. In cases where no other underlying cause or contributing factor may be attributed to for the occurrence of the patient’s Insomnia and all it’s associated symptoms, the diagnosis is therefore identified medically as psycho-physiological Insomnia, also known as primary Insomnia or alternatively, idiopathic Insomnia.

( Actigraphy Test – Image Courtesy of www.youtube.com )
Testing Insomnia
Insomnia may be tested and detected using Actigraphy lab testing which entails wearing an Actigraph upon the patient’s wrist or their ankle; measurements of decelerations or accelerations in their body movements are then taken as clear indicators of their sleeping or wakeful state.
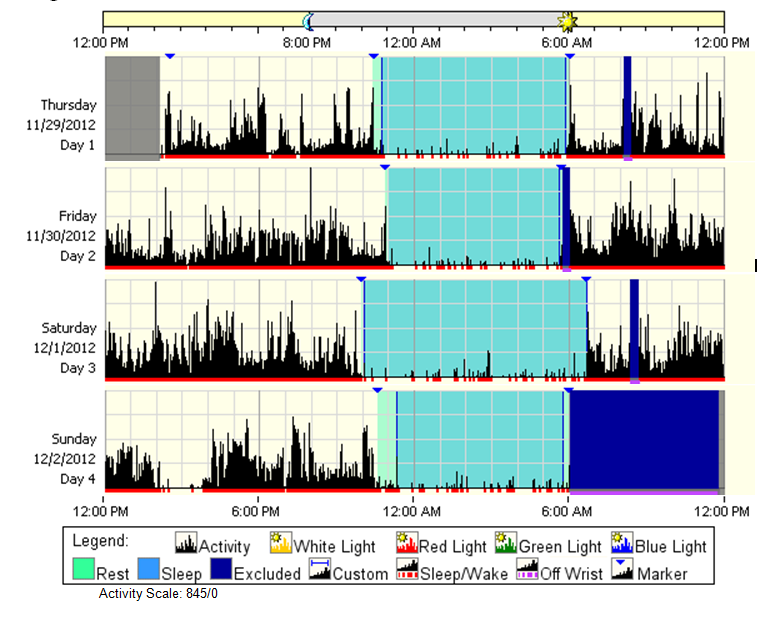
( Actogram in Actigraphy Testing – Image Courtesy of www.env-econ.net )
Conditions Linked to Insomnia
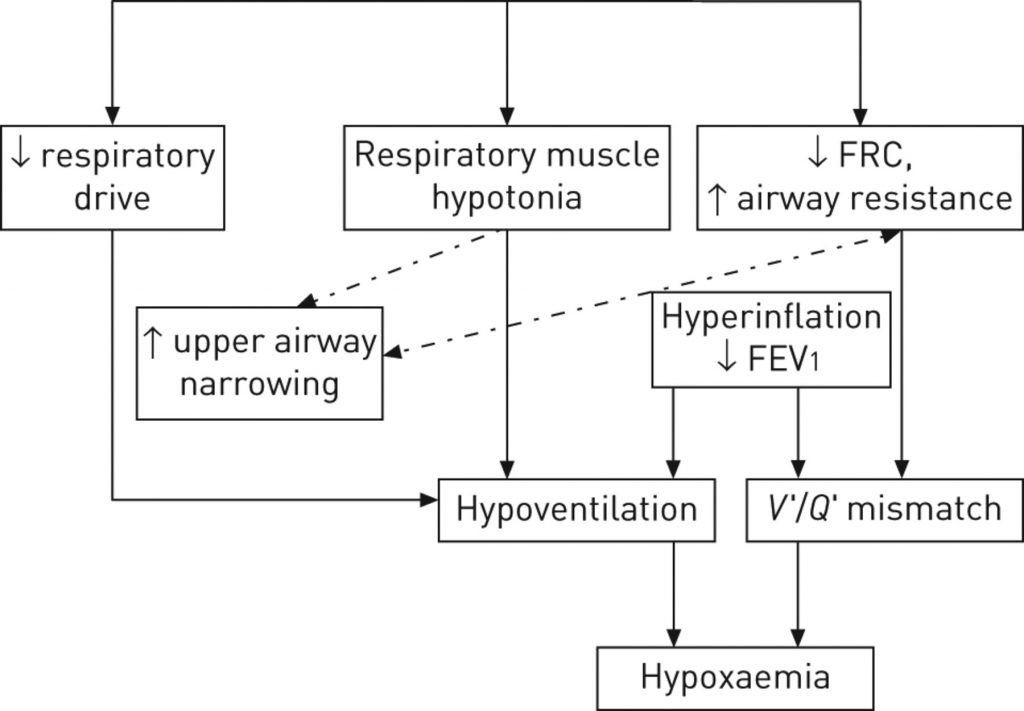
Medical professionals administering sleeping medication most commonly encounter cases of Insomnia in their practice. There are also various other sleeping disorders and medical conditions (psychiatric disorders and neurological conditions) associated with or that present Insomnia as a symptom, and careful testing, observation, and analysis should therefore be carried out for accurate diagnosis; this includes conditions such as: OSAS (Obstructive Sleep Apnea Syndrome), Anxiety and Mood disorders, ADHD (Attention Deficit Hyperactivity Disorder), Bipolar Disorder, PTSD (Post Traumatic Stress Disorder), as well as Depression.

( Sleep Deprivation – Image Courtesy of healthpromotion.caltech.edu )
Historical Scientific Research of Insomnia
Various scientific experiments have been shown to link Insomnia with stimulation of the brain’s preoptic region of the hypothalamus. This is one of the active regions of hypnogenic neurons for NREM sleep, the other active region being located within the brain’s medulla where the NTS (Nucleus Tractus Solitarius) is. The studies are based on the active stimulatory effects, ablations and lesions, and also recordings or the intracellular and extracellular activity of these brain regions.
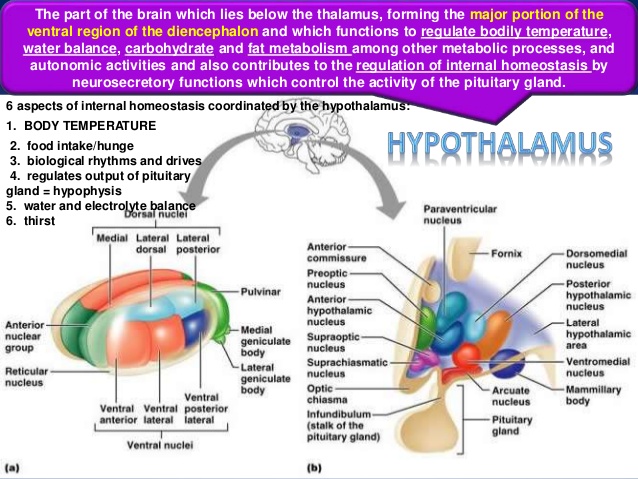
( The Hypothalamus – Image Courtesy of www.slideshare.net )
One such experiment, Batini’s, has proven the actively inhibiting function of The hypnogenic neurons of the brain’s lower stem on the brain’s upper stem. The behavioral sleeping state, as well as the synchronization produced by an EEG (Electro Encephalograph), both of which are produced by electrical stimulation of the brain’s preoptic area were also assessed in experiments by Nauta in 1946. Findings from Nauta’s experiments further elicited the onset or occurrence of Insomnia due to lesions present in the brain’s preoptic region. These findings would be later used to hypothesize the presence of actively working hypnogenic neurons within the brain’s preoptic region (in the forebrain). Later experiments in 1968 by Sterman and McGinty went ahead to confirm the findings from Nauta’s studies. Even so, not too long ago, further studies have gone to confirm that lesions of the ibotenic nature present within the brain’s preoptic area may also lead to Insomnia; thus further supporting the results that show the preoptic region as having a hypnogenic function that is active.

( Insomnia- The Hypothalamus and Homeostasis – Image Courtesy of wiki.bethanycrane.com )
Little Less Known Hypersomnia Sleep Disorder
Hypersomnia, a sleeping disorder that is related to Insomnia, involves complaints of EDS (Excessive Daytime Sleepiness), concentration problems, impaired motor abilities, poor cognitive function, and persistence of symptoms even after extended sleep at night.

( Hypersomnia – Image Courtesy of www.pinterest.com)
Lab testing such as pulmonary functional analysis may be done to assess the diagnosis of underlying Hypersomnia diagnosis.
( Pulmonary Function Analysis – Image Courtesy of err.ersjournals.com )
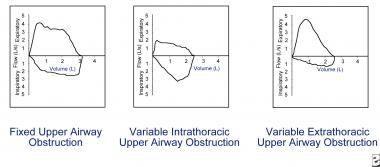
( Pulmonary Function Testing – Image Courtesy of emedicine.medscape.com )
Occurrence of Hypersomnia
Hypersomnia that occurs idiopathically (idiopathic Hypersomnia) without any other co-morbid conditions may be easily confused with Narcolepsy, another sleeping disorder which entails excessive sleepiness. Though it is yet to be proven, it is assumed that the cause of Hypersomnia originates from the CNS (Central Nervous System).

( Hypersomnia – Image Courtesy of chicagosleepcenter.com )
Testing Hypersomnia
Symptomatic Hypersomnia is typically syndicated with extended nighttime sleep (over 10 hours) or even normal sleep (about 6 to 10 hours): that is, Hypersomnia may occur with long sleeping time or without long sleeping time. These sleeping hours may be assessed by using sleep pattern history assessments, actigraphy, sleeping logs, and PSG (polysomnography) tests. Observations from the MSLT (Multiple Sleep Latency Tests) of Hypersomnia evidence admissible indications of pathological sleepiness but with the exception of sleep onset Rapid Eye Movement (REM).
Onset of Hypersomnia is usually seen around 15 to 30 years of age, which is much like the onset of Narcolepsy; however the two sleeping disorders differ in the nature of the sleeping pattern. In Hypersomnia, the patient is generally seen to sleep for many hours though the sleep is neither refreshing nor sufficient, nonetheless.

( Hypersomnia – Image Courtesy of www.utsleepdisorders.org )
Hypersomnia and EDS
Because Excessive Daytime Sleepiness (EDS) is another symptom of Hypersomnia, it may be easily confused with a misdiagnosis of Sleep Apnea. Therefore the patient needs to be further assessed for the following symptoms to rule out Sleep Apnea: frequent or intermittent awakening episodes all through the night, snoring, and cataplexy. Careful diagnosis should be made for many are the cases where Hypersomnia is misdiagnosed and confused for other conditions associated with EDS.

( Hypersomnia – Image Courtesy of healthysmart.org )
Various sleep experts have suggested the possibility of arbitrated by Cytokine proteins (like interleukin – specifically IL-6, and tumor necrosis factor – specifically TNF-α) in both Insomnia, and Hypersomnia that is idiopathic.
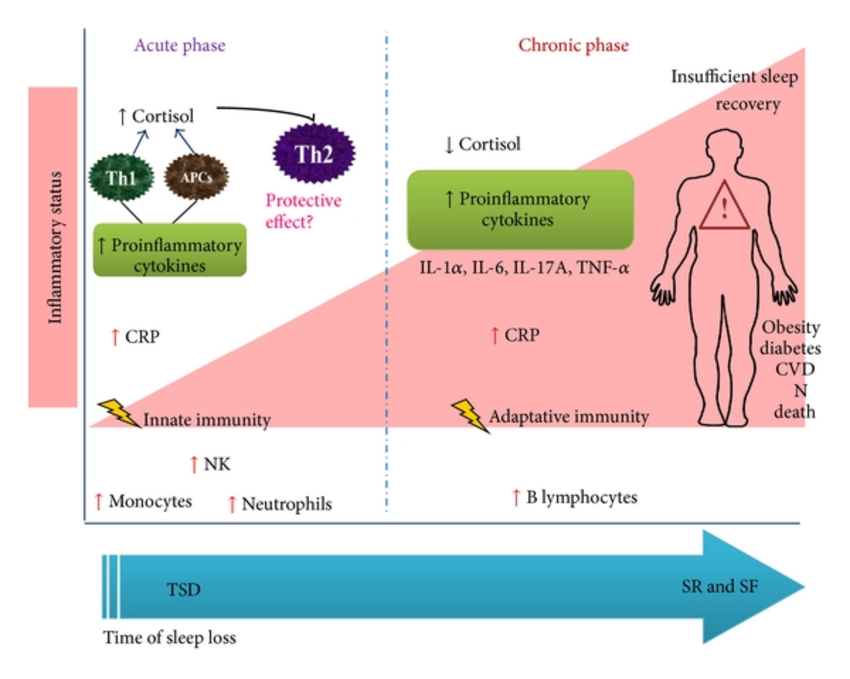
( Cytokines and Sleep Loss – Image Courtesy of www.researchgate.net )
It may very well be said of both Insomnia and Hypersomnia to be life-long chronic conditions that are disabling and lower the quality of one’s life. However, did you know that adjustable beds have helped many insomniac people fall asleep after many years. Check our our many adjustable bed reviews such as the Classic Brands adjustable bed review to see if it can help relieve your insomnia.

( Hypersomnia – Image Courtesy of www.americansleepmedicine.com )
