When their eyeballs are not squinting in beaming glare, they are often bloodshot from strain-among other complaints from sleep-disordered Americans. Their sleeping patterns and sleep problems seem to have synchronized with their work schedules and not their natural wake-cycle biorhythm. Lifestyles are adjusting their Circadian clocks like Daylight Savings Time (DST), regardless of the time-zone. Someone’s camera might just need to shutter, shut…maybe not Big Brother, but this could be you.
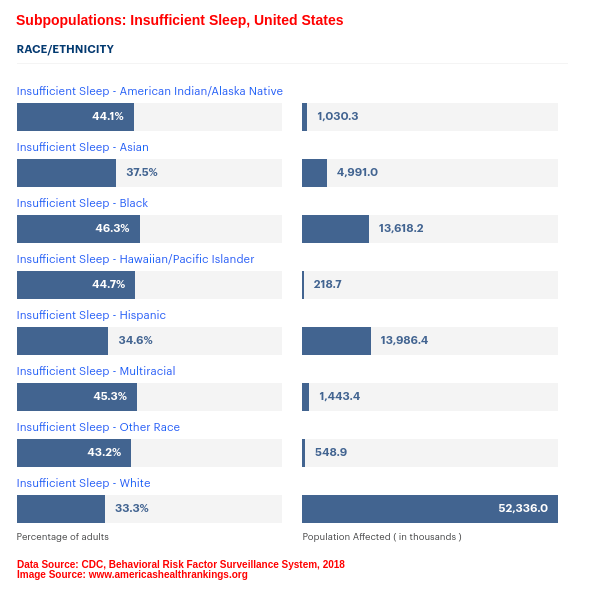
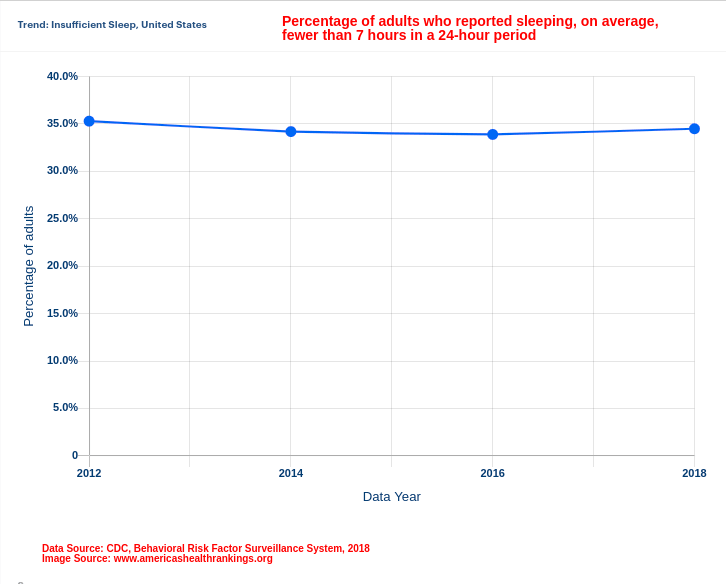
What are the odds that you were not 1 in 50 or 70 million Americans who in the year 2003[1] were chronically suffering from a sleep disorder? In most cases, headache, migraine, or facial pain could be the key reasons that can deprive a person of sleep. In the event that a person is suffering from craniofacial pain (pain related to the face and neck), going to a doctor’s clinic or physical therapy center might be helpful. If that was a sneeze from a snoozed timeout, then the serious bout is the 80 to 90 million Americans reported to have insufficient sleep by the year 2018. [2]. Albeit by a small margin, there were more Americans having inadequate sleep in the lower income bracket than in higher income brackets [2], perhaps money could indeed buy sleep… The bigger marginal difference was in the ethnic sleep profile, but not in gender parity. White Americans are 4 times more likely to have sleep loss than African Americans or Hispanics; but women sleeping less were just as much as the men who were. [2]

The sleep profile definition of an American living the typical lifestyle within any borders of the 50 states in the US highlights at least one of these complaints:
- Non-restorative sleep
- Early morning awakening
- Frequent nocturnal awakening
- Difficulty initiating sleep
- Difficulty maintaining sleep
Coupling their high prevalence in the US population is the inevitable interference of these sleep problems with optimal to normal functioning (role performance).
What’s Causing Sleep Loss in Americans
- Medication
- Comorbidities
- Headaches and Migraines
- Shift Working and Circadian Rhythm
- Sedentary, Inactive Lifestyle vs. Physical Activity
- Diet
- Age
- Stress
- Fatigue and Burnout
- Sleep Hygiene
1. Medication
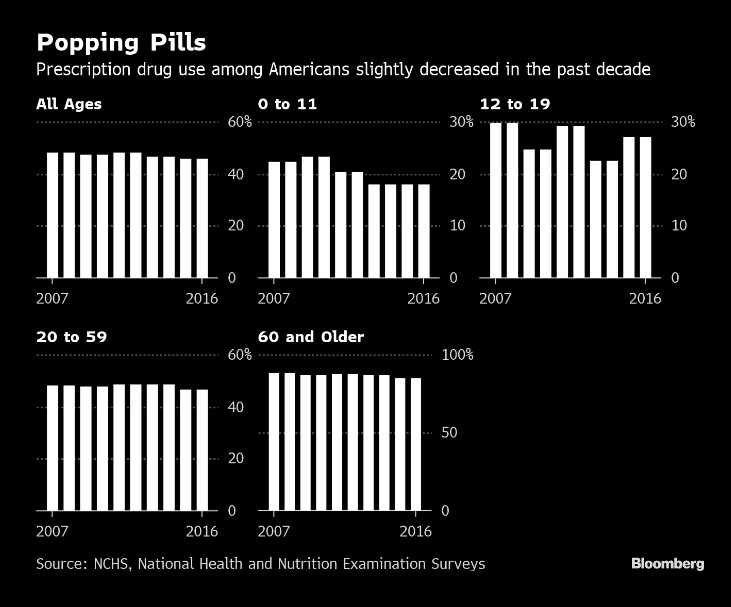
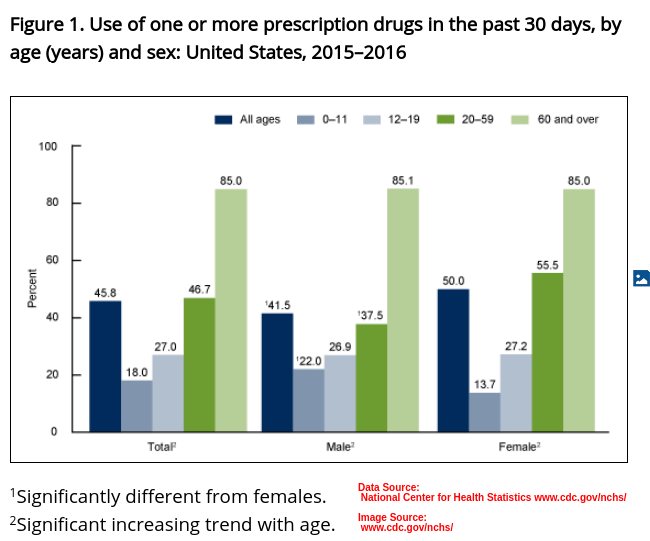
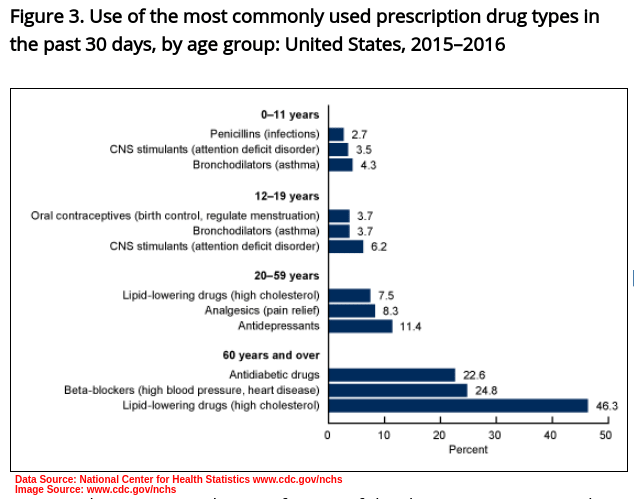
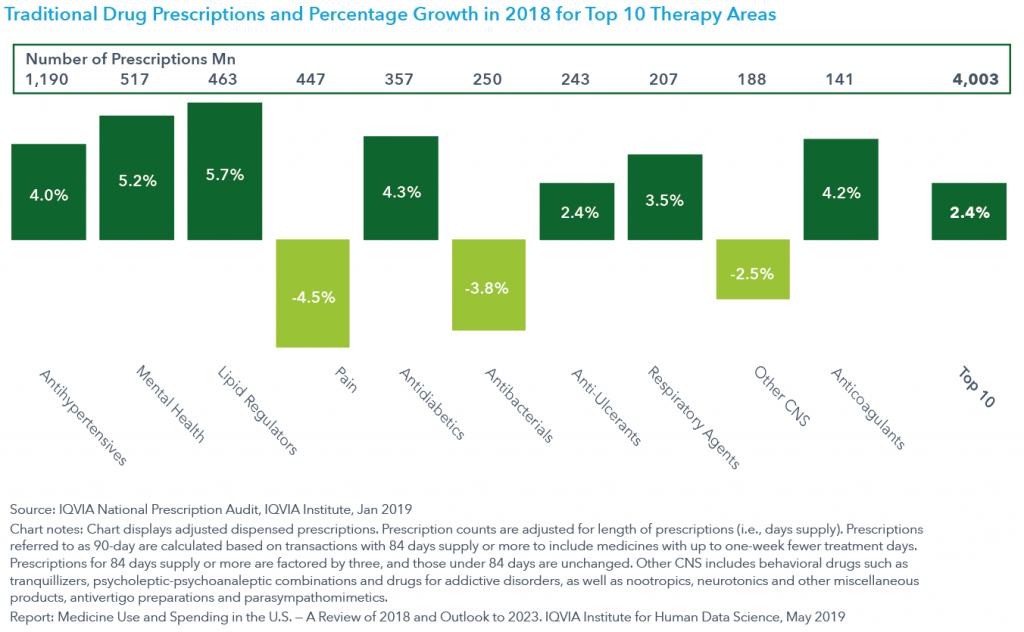
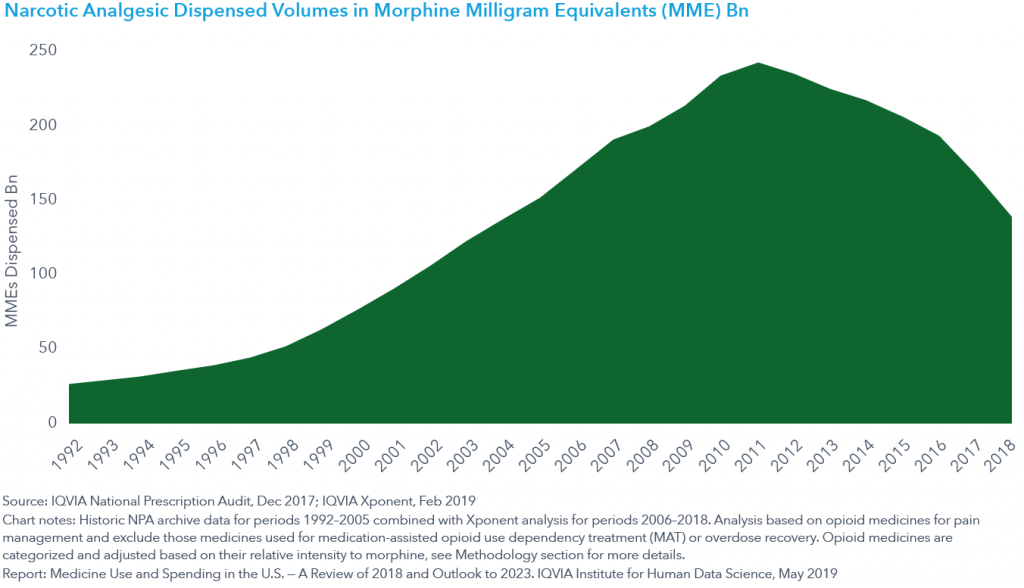
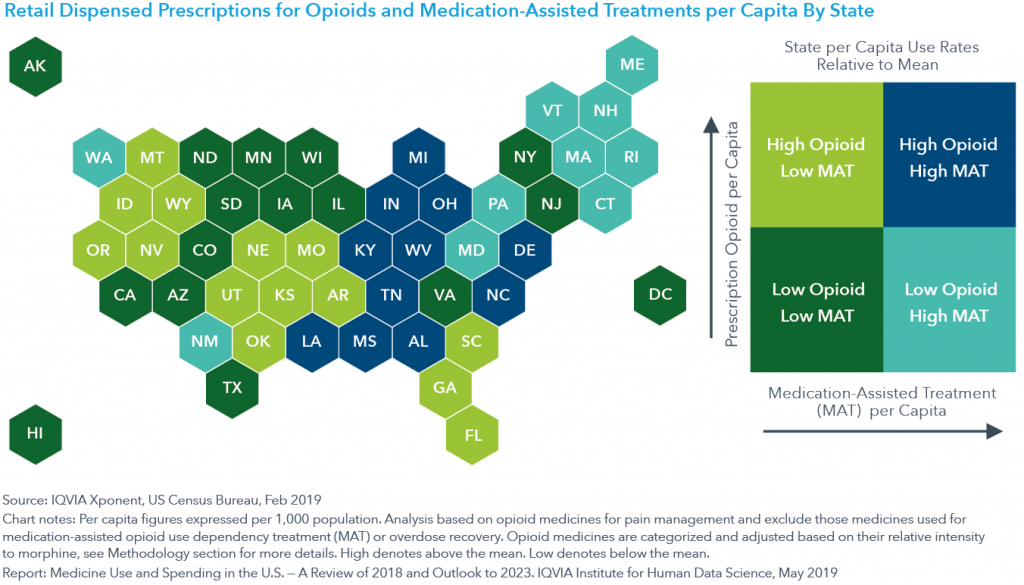
According to NCHS – National Center for Health Statistics data[3], as seen in 2015-2018, about 45.8% of the US population was on prescription medicine. Thus just about 1 in every 2 Americans is “popping pills”, you know, “taking something for it”. In year 2018 alone, 5.8 billion medical prescriptions were filled, an Year-over-Year increase of 2.7% compared to 2017.[4] The trend has not been much different in the previous decade, from year 2007 – 2016.[4]
Sleep Contraindication: Medication
Several factors linked to medication are contraindicated in sleep, i.e: sleep patterns, sleep cycle, sleep disorders, and sleep loss or sleep impairment. These are discussed below.
Chronic Pain
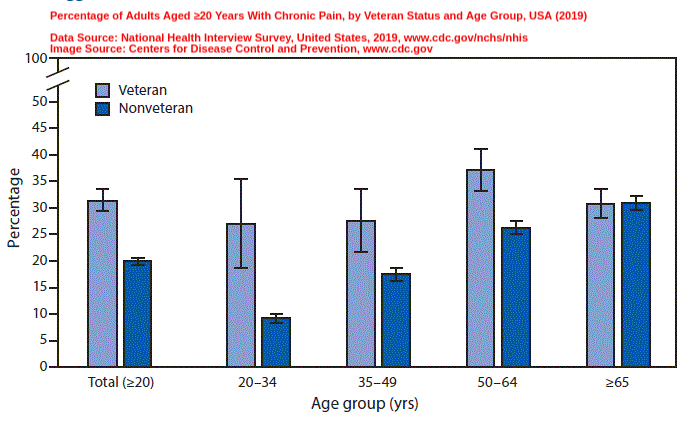
By the year 2016, Chronic pain in the US was shown to have a prevalence of at least 20.4%. That is at least 1 in 5 Americans were suffering from Chronic pain. An additional 8% were suffering from High-impact Chronic pain, according to statistics from NHIS (National Health Interview Survey).[6] Did you know that adjustable beds can relieve various types of pains, especially those related to age, trauma, and surgery?
By the year 2019, the percentages were roughly the same, with higher proportions of Chronic pain among veterans compared to non-veterans (31.5% to 20.1%). Chronic pain in non-veteran Americans was shown to increase with age.[6]
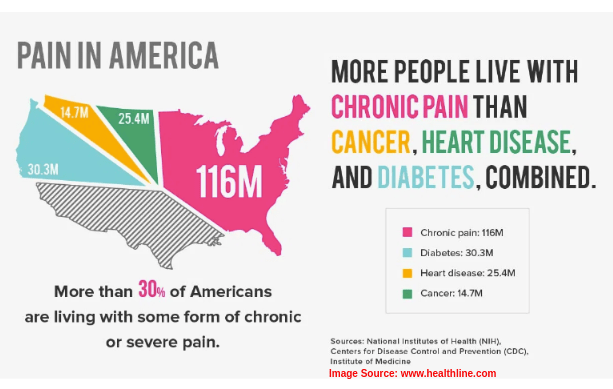
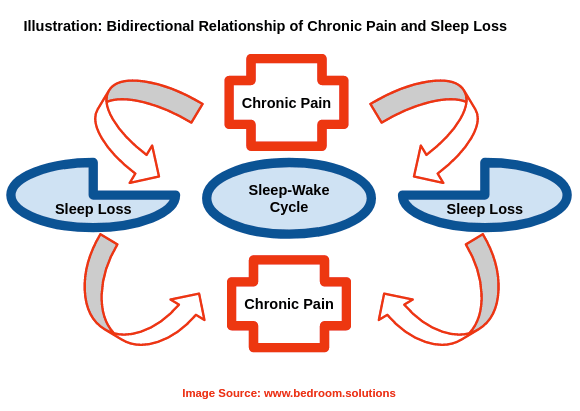
The association between chronic pain and sleep[7] is bi-directional in a vicious cycle that requires effectively treating both simultaneously.
- Patients with chronic pain also suffer from sleep impairment and wakefulness; studies have shown that 1 in every 4 chronic pain sufferers also has clinical Insomnia.
- Increased sleep disturbance lowers the chronic pain threshold; insufficient sleep directly correlates with chronic pain habituation.
- The sleep loss and sleep disruption experienced further aggravates the duration and severity or intensity of chronic pain.
- More than 70% of patients with chronic pain experience sleep deprivation which further causes the Hyperalgesia (hypersensitivity to pain stimulus).
- There is higher prevalence of Sleep Apnea in chronic pain patients taking opioid medication than in other patients taking long-term opioid medication, though untypical an effect of prescription opioids – opioid-induced Sleep Apnea.[8]
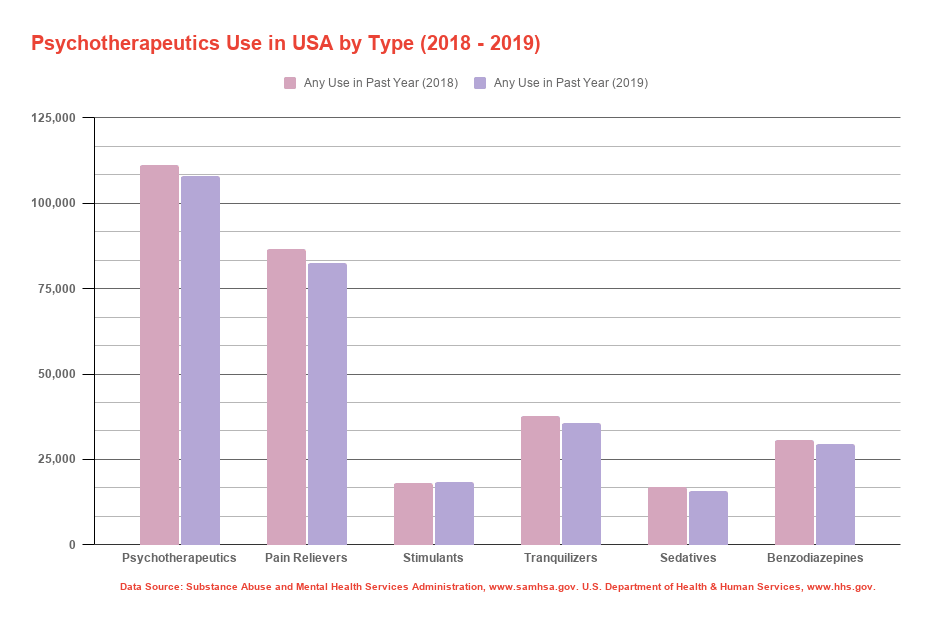
NMU and NMUPD
Not to be confused with “drug abuse” the prevalence of Non-Medical Use (NMU) of Prescription Drugs (NMUPD) is just as rampant in the US, particularly in the 18 – 25 age group.[11]
Research indicates 5 aspects of Sleep Quality that are affected by Non-Medical Use (NMU) of Prescription Drugs (NMUPD):
- Daytime Sleepiness
- Difficulty Falling Asleep
- Early Awakening
- Enough Sleep
- Problem with Daytime Sleepiness
Main motivations identified for Non-Medical Use (NMU) of Prescription Drugs (NMUPD) include:
- High Performance Pressure (in academic institutions, at workplaces).
NMUPD stimulants are used for wakefulness, alertness, and delayed sleep.
- Self-Esteem boost (raising confidence levels).[11]
- Addiction and Withdrawal from substance use (due to abuse and misuse).[11]
- Off-Label supplementation (for desired results or drug side-effects).
Sleep problems associated with NMUPD of stimulants and of painkillers[9] are:
- increased days of Early Awakening – Sleep Disturbance
- decreased days of Enough Sleep – Sleep Duration
- increased Difficulty Falling Asleep- Sleep Latency
- Increased Daytime Sleepiness – EDS, Excessive Daytime Sleepiness
Sleep problems associated with NMUPD of sedatives[9] are:
- increased days of Early Awakening – Sleep Disturbance
- increased Difficulty Falling Asleep- Sleep Latency
- Problem with Daytime Sleepiness – poor Sleep Quality
Sleep changes associated with NMUPD of antidepressants[9] are:
- improving Sleep Architecture
- reduction of REM (Rapid-Eye Movement) Sleep Onset Latency
- Increased REM sleep
- short-term increased Sleep Disturbance (e.g. some Selective Serotonin Receptor Inhibitors (SSRIs)
- long-term increased Sleep Quality (e.g. some Serotonin 5-HT2 receptor antagonists)
- some cases of Insomnia and of EDS, Excessive Daytime Sleepiness
Covid-19 Update: Medication
With Covid-19 high-risk demographics being the elderly and those suffering from chronic comorbidities, the same group has a high prevalence of chronic pain (CP)[10], and are thereby long-term users of pertinent medication for CP.[10]
2. Comorbidities
Various comorbidities that are majorly linked to sleep problems in the US include:
- Mentall Illness (Depression, PTSD – Post-Traumatic Stress Disorder, Major Anxiety Disorder, Alzheimers Disease)
- Cancer
- Fibromyalgia
- CFS – Chronic Fatigue Syndrome
- Endocrine Problems (Hormonal Imbalance, Metabolic Disorders)
- TBI – Traumatic Brain Injury
- Headaches and Migraines
- Hypertension
- Heart Disease and Stroke
- Diabetes
- Kidney Disease
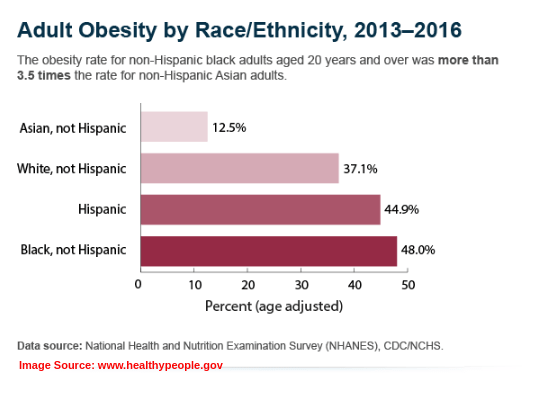
- Obesity
- Respiratory Diseases
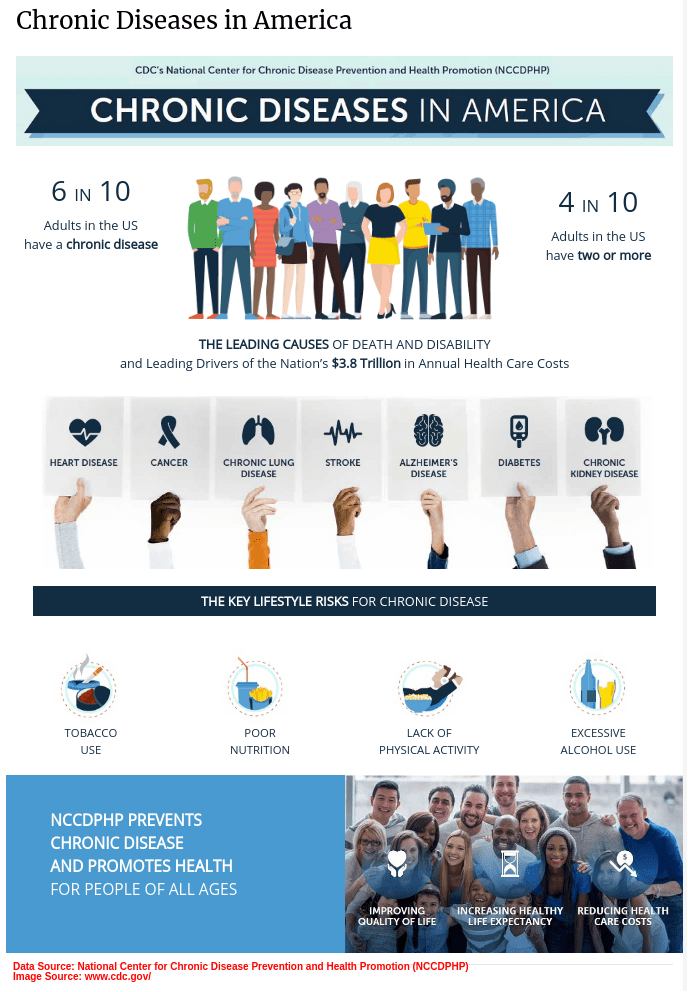
These comorbidities are also chronic conditions, and they affect about 1 in 2, i.e. about 45% or approximately 133 million Americans, with a trend that’s been growing through the years.[12] The CDC (Centers for Diseases Control) indicates that they account for about 75% of the healthcare costs incurred by Americans.
Sleep Contraindication: Comorbidities
Mental Illness: Depression, Anxiety
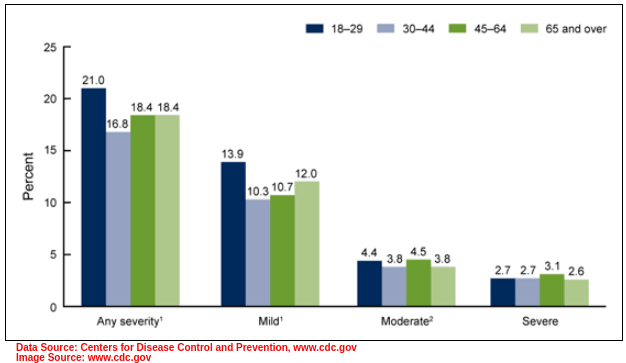
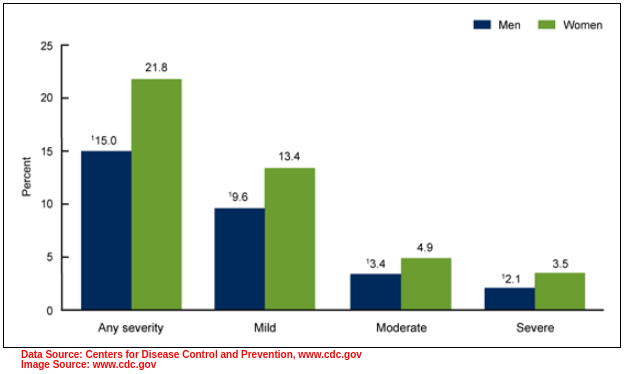
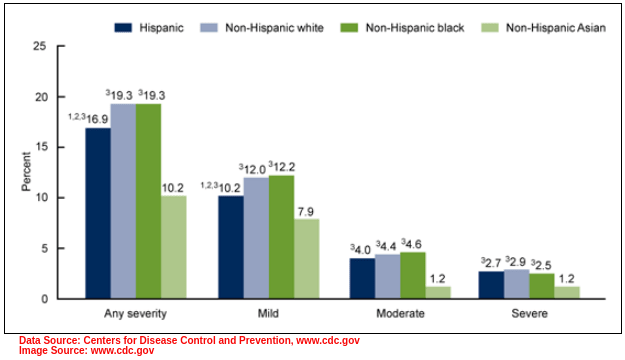
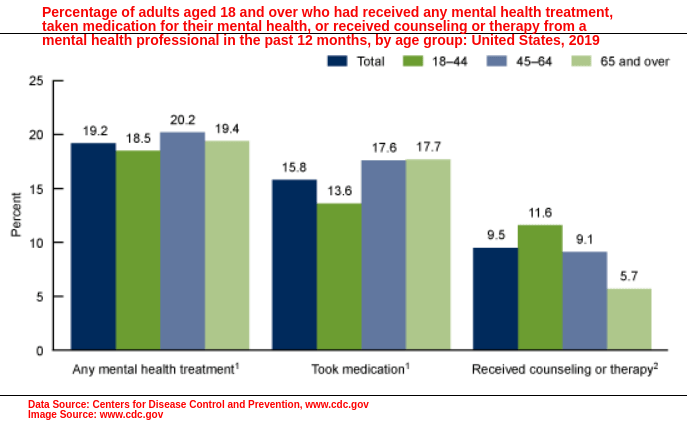
Epidemiological indicators for Depression (MDD – Major Depressive Disorder) and Anxiety (GAD – Generalized Anxiety Disorder) are contraindicated and have been on the rise in the past two decades. Short-term MDD and long-term MDD prevalence ranges from 10.4 – 20.6% respectively[13] [14]. Generally affecting the age groups (in percentages): 21% (18-29 years); 18.4% (45-64 years); 16.8% (30-44 years).[13] [14]
Sleep problems are associated with Anxiety and Depression, as seen in about 73.4% of diagnosed patients. It’s a bidirectional and directly proportional relationship with Sleep-Wake disorders presenting sleep difficulty, sleep disturbance, and affecting sleep quantity, sleep quality in the DSM-5 classification. The symptoms are:[15]
- Difficulty initiating sleep
- Difficulty maintaining sleep:
- Persistent, frequent Insomnia(oset of Insomnia, maintained Insomnia, mixed Insomnia);
- Increased awakenings(Sleep Disruption)
- Early awakenings: with difficulty returning to sleep
Further, compared to Caucasians, African Americans were 3.4 and 4.8 times more prone to having (respectively) clinical MDD and GAD; and women more prone than men.
The inverse also applies bidirectionally, in that Insomniais a diagnostic criterion or a risk factor leading to clinical Depression.[16] Patients with exclusive Depression are 6.7 times more likely to develop Insomnia later on in life. It’s been proven scientifically; the comorbidity of Mental illness (MDD and GAD) with Insomnia and other sleep disorders remains unrefuted.[16] Sleep problems are a precursory symptom (prodromal) and not a secondary side-effect (epiphenomenon) of Depression, contrary to what was initially indicated.[17]
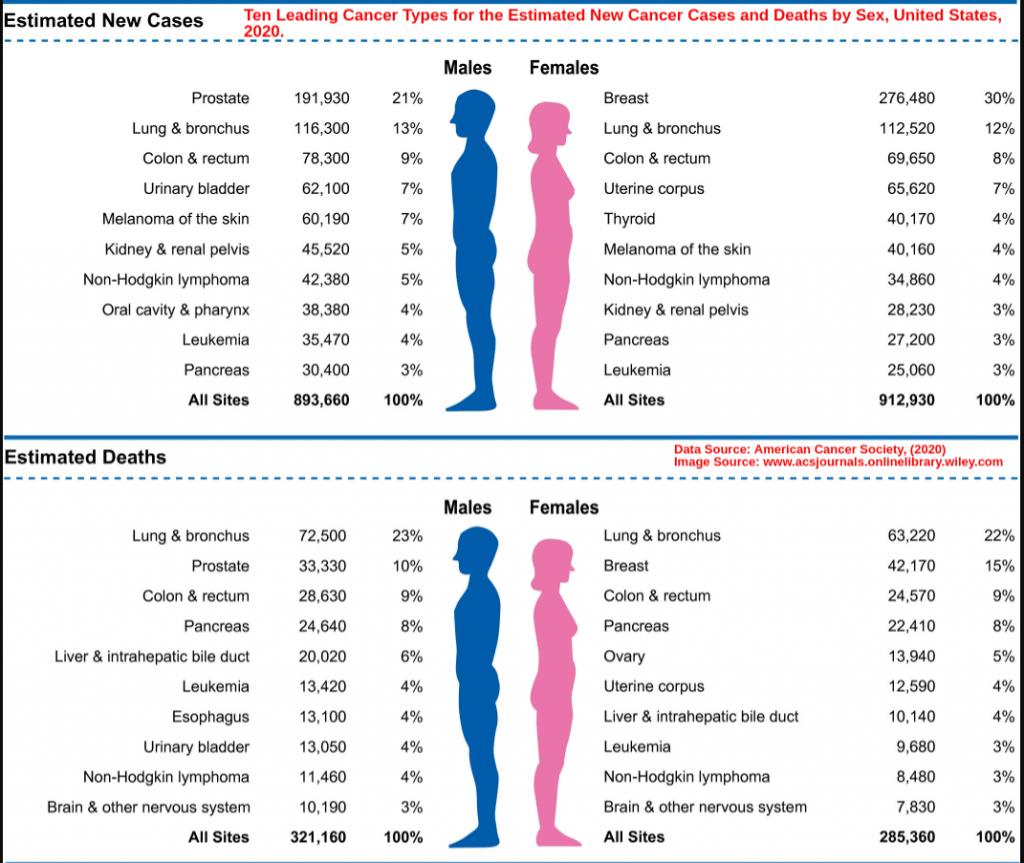
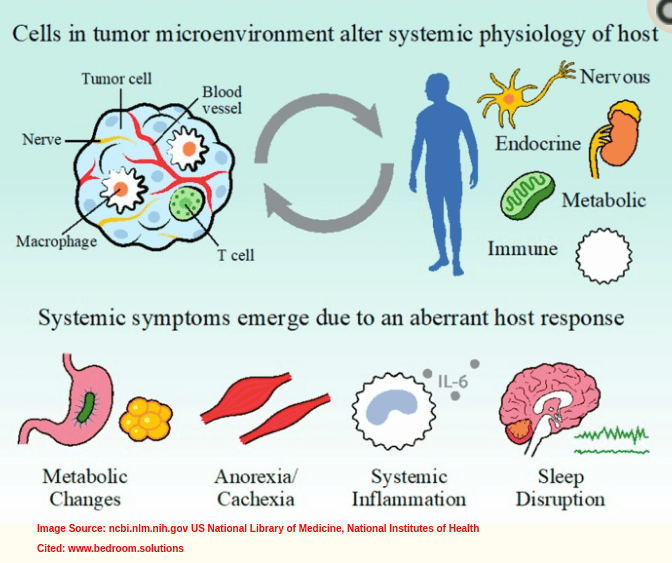
Cancer
Sleep contraindications in Cancer patients are 2 times more than in the general population, according to a National Cancer Institute assessment. The Cancer-induced sleep problems, which could be prolonged for years after Cancer treatment, mainly entail:
- Sleep-Wake disorders (difficulty initiating sleep, and maintaining sleep)
- Circadian Rhythm disorders (biological clock affecting the Sleep-Wake cycle)
Sleep problems were reported in about 59% of over 13 million Cancer survivors.[17] By the year 2019, Cancer survivors The 2017 – NHIS, US National Health Interview Survey, showed that prevalence was in:
- Gender: Female
- Age group: 40 years and above
- Race: White non-Hispanics
There has been marked improvement in sleep disruption experienced by Cancer survivors and Cancer patients using alternative MBM (Mind-Body Medicine) therapy.[17]
Cancer-induced sleep problems in Cancer patients and Cancer survivors manifest as the following symptoms which lead to increased mortality and poor quality of life:[18]
- Circadian Dysrhythmia (disruption of sleep patterns)
- Hot Flushes (hormonal imbalance)
- Hypersomnia
- Insomnia
- Nightmares
- Somnolence Syndrome (drowsiness, impaired cognition, lethargy, poor performance)
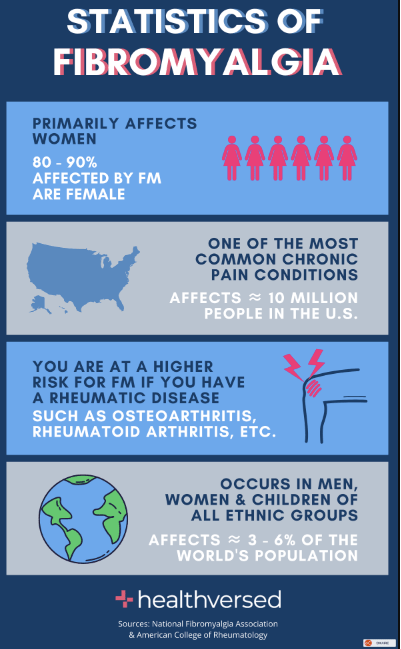
FM – Fibromyalgia
The chronic condition, FM, Fibromyalgia, has the typical symptoms of chronic pain and mechanical Hyperalgesia. NHIS – National Health Interview Survey statistics showed that it affected about 4 million Americans, i.e. approximately 1 in every 50 Americans had Fibromyalgia in the year 2010.[19] More recent figures from the NFA – National Fibromyalgia Association stand at no less than 10 million Americans living with Fibromyalgia,

Women are more prone to having Fibromyalgia, taking up approximately 75-90% of the affected population.Targeted demographics are the 30-60 age group, and by 80 years of age, about 1 in every 12 seniors (8%) is affected by Fibromyalgia.
Studies have shown the prevalence of Insomnia to be higher by 50% -80% in patients with Fibromyalgia as compared to 10-15% of patients without it.[20] Reports of sleep discrepancy were imminent (i.e. discrepancies in self-reported sleep problems compare to objective measurements of sleep). It is a biredirectional linkage that correlates to Chronic Pain as herein discussed. Sleep Discrepancy, which is closely linked with Paradoxical Insomnia is the state in which the individual is “paradoxically asleep”: active brain EEG, Actigraphy REM-sleep activity, energy consumption, but with the body in complete inactivity.[20]
CFS/ME – Chronic Fatigue Syndrome/ Myalgic Encephalomyelitis
Chronic Fatigue Syndrome/ Myalgic Encephalomyelitis (CFS/ME) is a debilitating and complex disease which causes fatigue, lethargy, pain, poor performance and sleep disruption. It is exacerbated with strain (or “exertion”). and is prevalent in women.[21] It is presented as CFS/ME in adults and Pediatric CFS/ME.
Contrary to the notion: CFS is a “women’s disease” (due to its prevalence), it does not exclusively affect women. There are at least 2.8 million to 3.38 million Americans affected (i.e roughly 857 in every 100,000) in total. Research shows that the US demographics affected by Chronic Fatigue Syndrome are as highlighted below:[22]
- Women: The ratio of men to women with CFS can go up to 1:4
- Men: About 35-40% of CFS/ME diagnoses affect men
- Children: Pediatric CFS is less prevalent than adolescent CFS
- Adolescents: Those affected range from 0.11% to 4% of adolescents with CFS
- Elders: Highest CFS prevalence is in the age group of 40 – 60 years

Individuals with ME/CFS, which was renamed to Systemic Exertional Intolerance Disease (SEID), oftain complain of these symptoms (which are also diagnostic criterion for ME/CFS):[23]
- Non-restorative sleep
- Non-refreshing sleep (tiredness in the Wake Cycle as is experienced prior to the Sleep Cycle)
- Insomnia (difficulty initiating sleep, frequent or prolonged Nocturnal Awakenings, early-morning awakenings, EDS -Excessive Daytime Sleepiness )
- Hypersomnia
- Sleep disturbances:
- Hypnogic jerks (also called “sleep starts” or Myclonus)
- PLMS – Periodic Limb Movement Syndrome
- RLS – Restless Leg Syndrome
Only a small fraction of CFS/ME/SEID patients do not experience some form of symptomatic sleep dysfunction. Sleep metrics like Actigraphy have shown that there are circadian rhythm disruptions observed in people with ME/CFS[24]. The Circadian clock controls, among other functions, the sleep-related functions of: Sleep-Wake cycle, Alertness-Tiredness. Dysregulation of the circadian rhythm could in fact be used in CFS/ME diagnosis as a concomitant symptom.
Yet another contributing factor to sleep problems in CFS/ME is the resultant decrease in pre-frontal cortex GM (gray matter) which causes sleep dysfunction.[25]
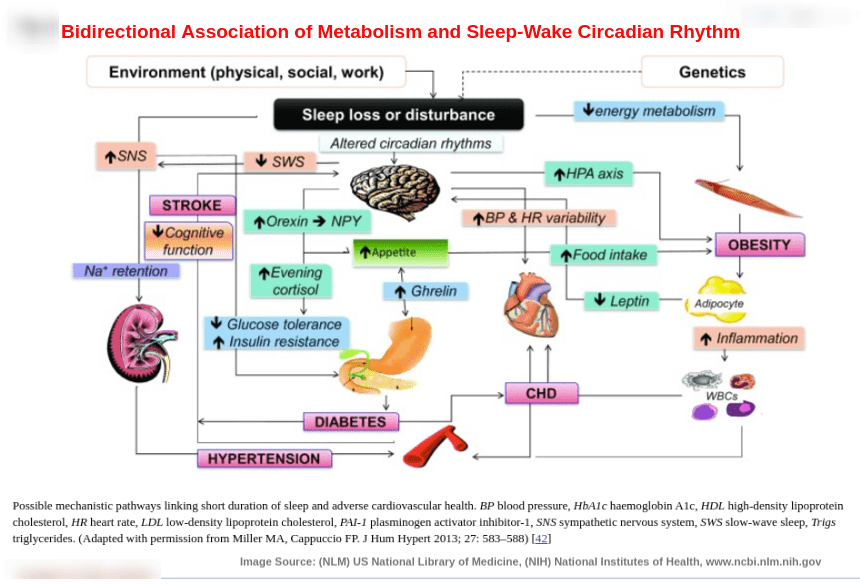
Endocrine Problems: Hormonal Imbalance and Metabolic Disorders
Disorders of the Hypothalamus-Pituitary-Axis (HPA) greatly affect sleep as it regulates the Circadian Sleep-Wake Cycle, which governs the endocrine biorhythm of the “biological day and night”. HPA is one among the most crucial hormonal pathways for sleep regulation in the body. Thus the increase and fluctuation of hormones such as the sleep hormone Melatonin, the growth hormone Somatotropin, the stress hormone Cortisol, and the mood hormone Serotonin directly influence the sleep patterns, and vice-versa.[26]
The HPA affects the following sleep phases:
- REM Sleep (Rapid Eye Movement)
- SWS Sleep (Slow Wave Sleep)
Sleep-related endocrine functions of the HPA include stimulation of the Corticotropin Releasing Hormone (CRH) which promotes:
- Increased wake-time (Reduced wake-time is caused by CRH receptor antagonists)
- Increased Light phase (daytime, Wake cycle) hyperactivity of the HPA
- Onset of Insomnia (due to increased HPA activity and increased Cortisol secretion in the Light phase – daytime, Wake cycle)
Melatonin is the predominant hormone in sleep regulation. A function of Melatonin is in Circadian modulation, by stimulating sleep in the Dark phase of the Sleep-Wake cycle. It facilitates for the following:
- initiating sleep onset
- promoting sleep maintenance
- increasing total sleep time
Sleep dysregulation would arise from irregular signalling of the HPA. This is due to disrupted synthesis of Serotonin which in part contributes to the Circadian Rhythm.
Sleep loss is shown to be increased by low Testosterone and Testosterone HRT (Hormone Replacement Therapy) in men.
Decreased REM sleep coincides with high Estrogen and high Progesterone in women.
Increased SWS sleep correlates with production of Prolactin (in Hyperprolactinimea).
Sleepand stress bidirectionally influence each other as they share various CNS (Central Nervous System) pathways with metabolism. Sleep acts as a regulator of neuroendocrine functions and in glucose metabolism. Sleep problems that are interlinked or contraindicated in Metabolic disorders (such as Diabetes, Obesity) include:[27]
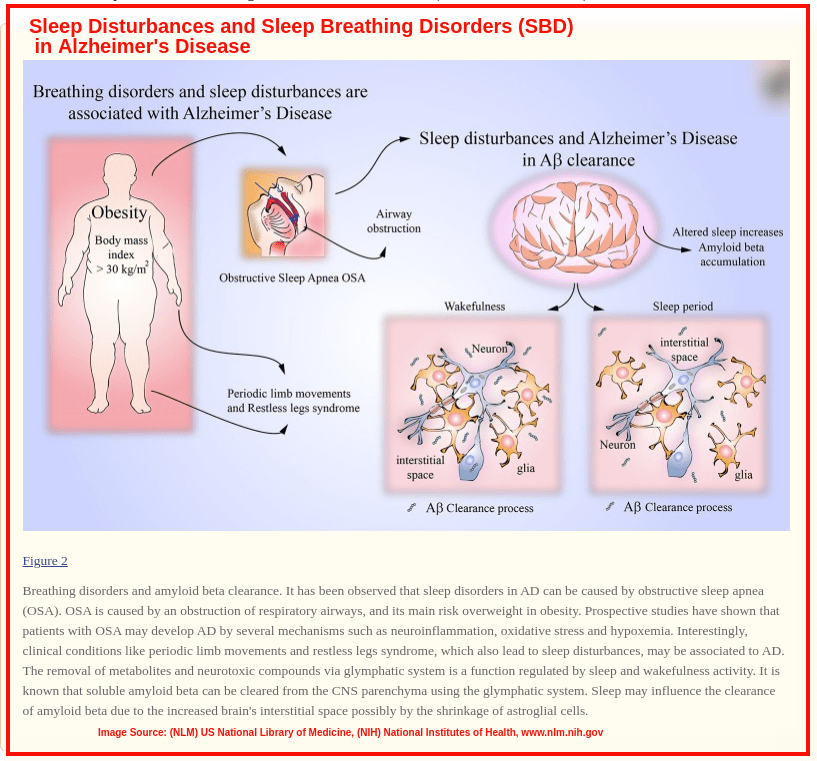
- OSAS (Obstructive Sleep Apnea Syndrome) – sleep and OSAS is contraindicated due to common ANS (Autonomic Nervous System) and CNS pathogenic pathways.
Obesity[27][28][29] is shown to be a causative factor of OSAS. It is also linked to short sleep duration (5-6 hours, or less)with a 25% more probability than long sleep duration (7-9 hours or more).
Diabetes[27][28][29] (Type II Diabetes mellitus) is also linked with OSAS due to its metabolic role in insulin resistance and glucose intolerance. It is also linked with: difficulty initiating sleep, and difficulty in maintaining sleep. Those affected may benefit by using the best berberine supplement, which is said to lower blood sugar levels. When the problem is under control, normal life can be achieved, which also includes a proper sleep pattern.
The bidirectional interplay between sleep and metabolism is influenced by sleep loss (due to poor sleep quality) with:
- decreased levels of appetite-suppresing hormone Leptin
- increased levels of hunger hormone Ghrelin
- increased appetite
- Increased hunger
- decreased insulin sensitivity
- decreased glucose tolerance
- increased evening Cortisol concentrations
Women with PCOS (Polycystic Ovarian Syndrome)[30]have higher risks of presenting difficulty initiating sleep, and difficulty in maintaining sleep, among other sleep problems compared to other controls and obese subjects in the studies:
- restlessness and restless sleep
- unrefreshing sleep
- unrestorative sleep
- sleep efficiency
- delayed sleep-onset latency
- REM sleep time (Rapid Eye Movement)
- NREM sleep time (Non-Rapid Eye Movement)
TBI – Traumatic Brain Injury
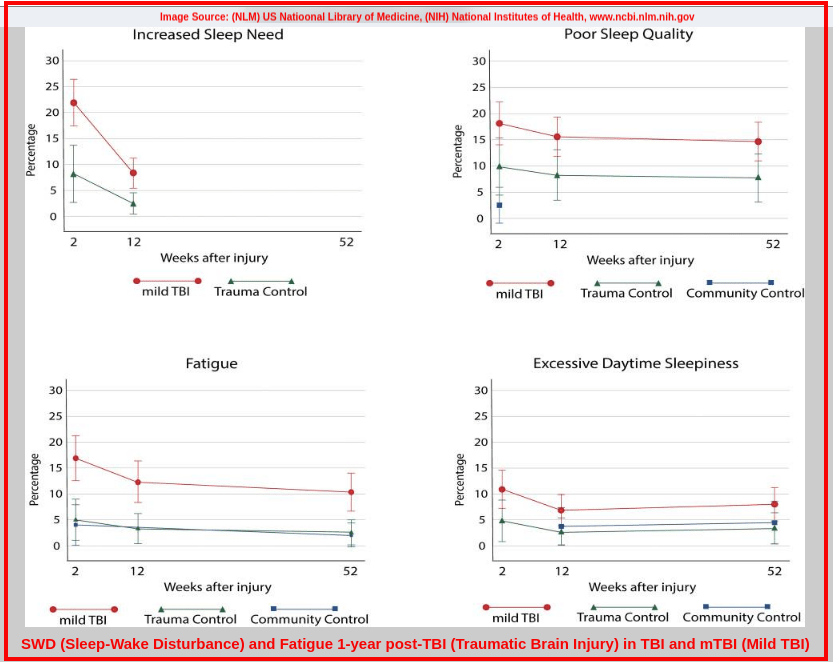
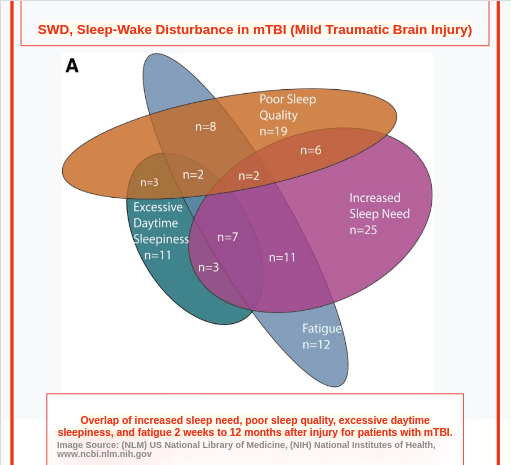
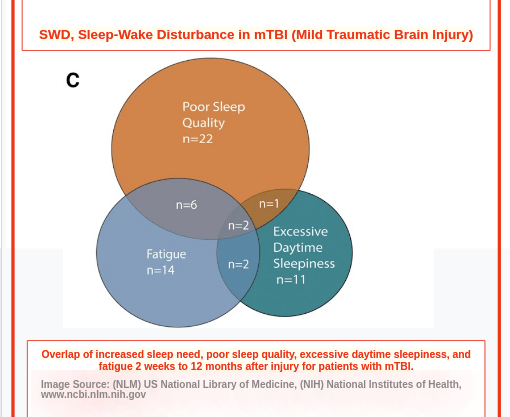
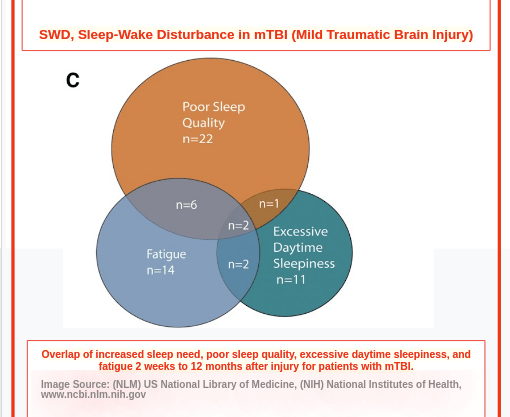
More than 2.5 million cases of TBI (Traumatic Brain Injury) are reported annually in America, most of them being mTBI (mild Traumatic Brain Injury).[31] These mostly arise from car accidents, violence and falls.
Studies supporting the incidence of Traumatic Brain Injury with disruption of Circadian Rhythm abound.[31][32][33] Reported sleep problems (SWD – Sleep-Wake Disturbance) have been reported in about 50-70% of TBI patients and these include:
- Sleep-Wake Disturbance (SWD): this can develop in the post-TBI (acute phase, subacute phase, chronic phase)
- Insufficient sleep
- Excessive Daytime Somnolence (EDS)
- Delayed Sleep Onset Latency (SOL)
- Poor Sleep Efficiency ( = total time asleep / total time in bed)
- Difficulty initiating sleep
- Difficulty maintaining sleep
- Reduced Total Sleep Time (TST)
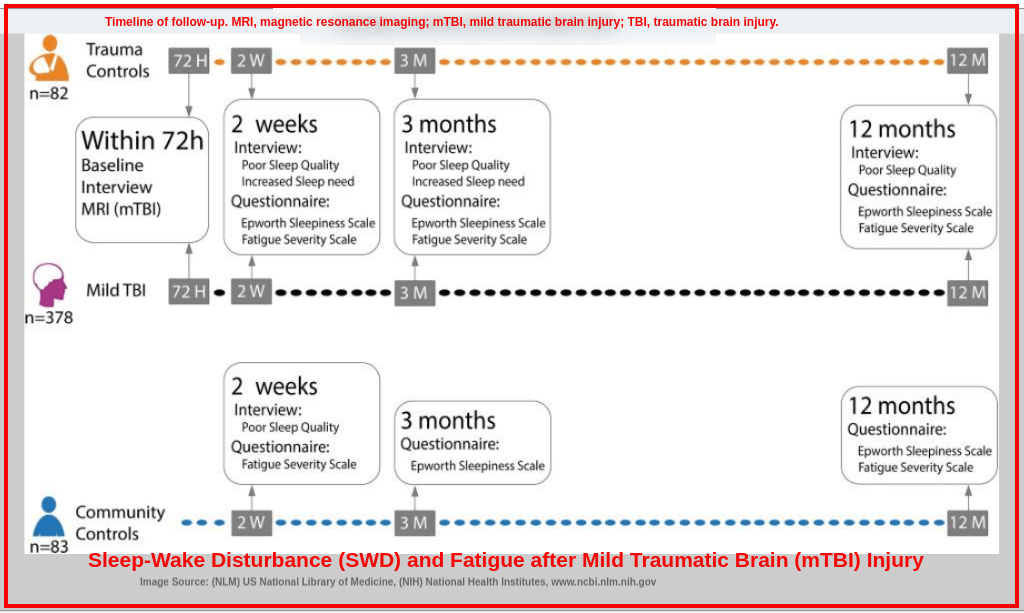
The main sleep sequelae associated with Traumatic Brain Injury are fatigue (daytime distress), Insomnia and Hypersomnolence.[31][32][33]
Patients with mTBI mostly complain of Insomnia:
- increased need for sleep
- unsatiating sleep
- poor sleep quality
- prolonged Sleep Onset Latency (SOL)
- increased Wake After Sleep Onset (WASO) – wake time after initial sleep and before final awakening
Patients with moderate TBI and severe TBI, (experienced in about 50-85% with remittance and persisting in about 10-53% without remittance),mostly complain of Hypersomnolence (Hypersomnia):
- excess sleep quantity
- Excessive Daytime Sleepiness, EDS
Should the Sleep-Wake Disturbance (SWD) persists over time in the post-TBI phase,clinical sleep disorders that could potentially arise are:
- Post-Traumatic Hypersomnia (PTH)
- Post-Traumatic Narcolepsy (PTN)
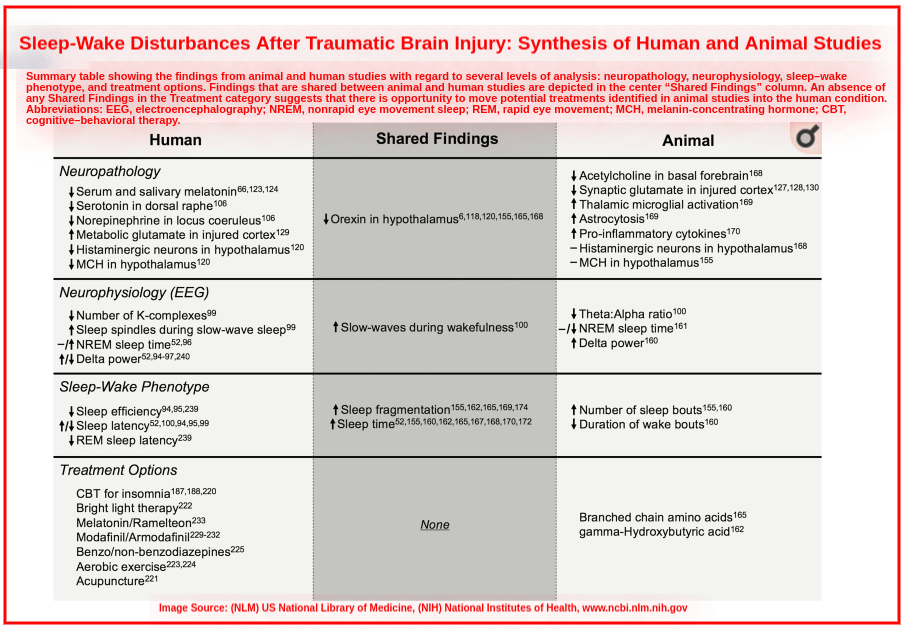

Traumatic Brain Injury (TBI) and sleep are bidirectionally interlinked in that:[31]82
Prognostic sleep loss (sequelae)due to TBI or mTBI further accelerates, exacerbates and/or prolongs:
- Neurodegeneration
- Long-term mTBI sequelae (including relentless sleep problems, disrupted Circadian biorhythms, Chronic Pain, PTSD – Post-Traumatic Stress Disorder, Depression, Anxiety, Cognitive dysfunction, protracted healing in repair and regeneration, among other complications.)
- Morbidity
3. Headaches and Migraines
Used as a diagnostic criterion[35] for most sleep disorders, headaches (Cephalalgia) affect about 50-75% of the population according to WHO (World Health Organization) statistics. Just about half the population, 1 in 2 individuals, having sleep impairment. It is no wonder that sleep and headaches are bidirectionally correlated and have acquired the “global health burden” status.[35]
In the GBD – Global Health Burden Study 2019[34], Migraineswere listed as a “disabling disease”, ranking 2nd among 369 diseases causing disability in individuals aged 50 and below. It is a neurological disease whose symptoms are completely debilitating. GBD 2019 reported thatglobally, at least 41 million migraineurs were affected in YLD’s – Years Living with Disability. Demographically, migraines most affect women and productive adults. The Migraine Research Foundation indicates that there are about 39 million migraneurs in the US (men – 6%, women – 18%, and children – 10%), approximately 12% of Americans, and more than 1 billion worldwide. About 1 in every 4 households in America has a migraneur.[34]
Sleep Contraindication: Headaches and Migraines
The Hypothalamus is the main link (pathophysioology) between headaches and sleep problems as it is the modulator of all sensation and the pacemaker of Circadian Biorhythms. Both sleep and headache have:
- many neurotransmitters, pathways and structures that are mutual and localized in the brain[35]
- a bidirectional correlation, a vicious circle[35]
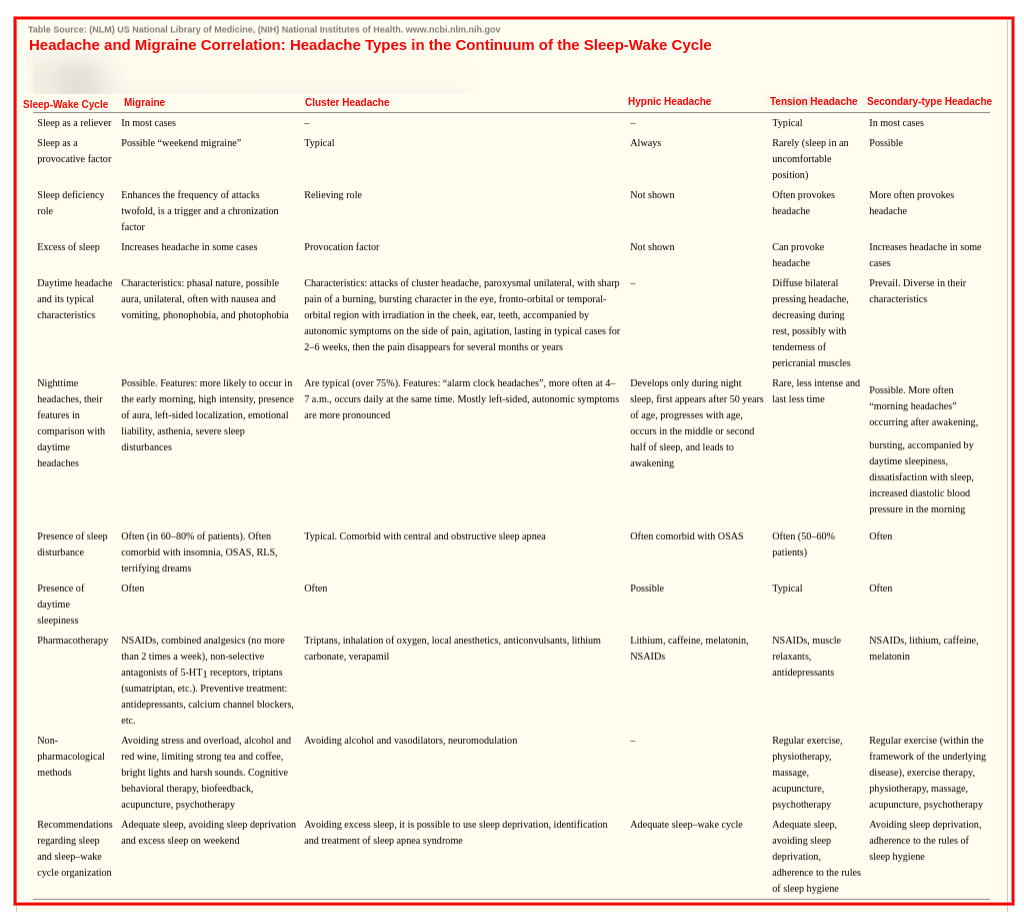
Pain aggravates sleep impairment, and raises stress levels. Individuals with persistent, chronic headaches and migraines are predisposed to:
- Sleep Disruption (during episodes of pain, wakefulness, alertness)
- Sleep Loss (due to bouts of pain, with increased use of sleep aids: sleeping pills, antidepressants, analgesics)
- EDS – Excessive Daytime Somnolence

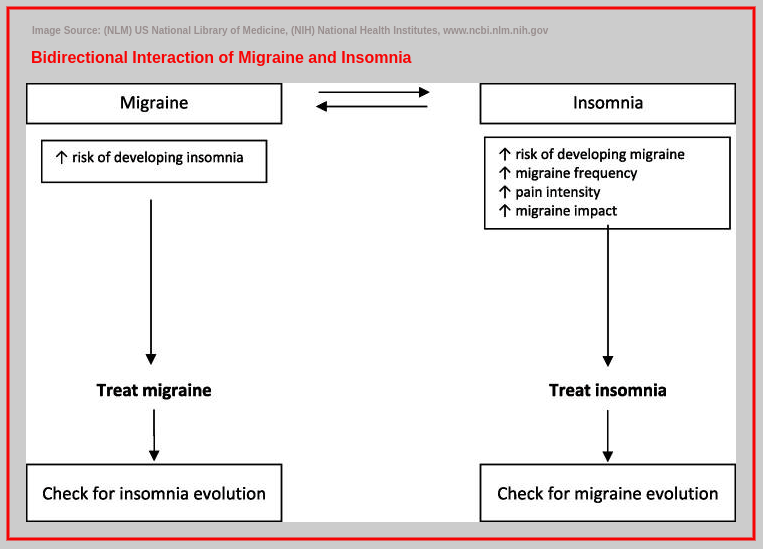
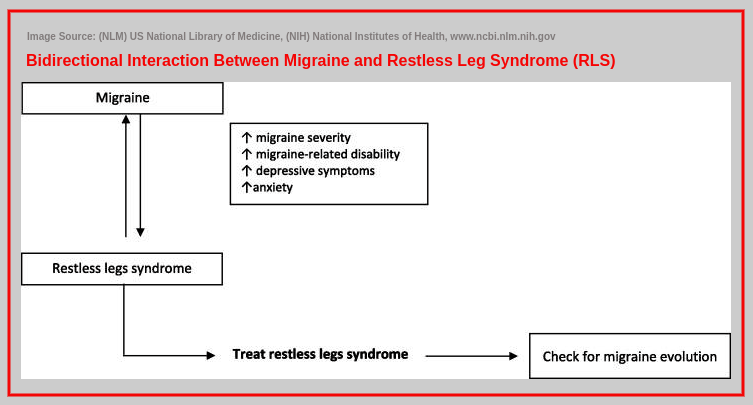
In a vicious turn, the sleep disturbances cause migraine triggers and consequently lower migraine thresholds. This exacerbates and complicates the headache and migraine pains through migraine chronification, catastrophization and dramatization. This further increase the predisposal to depression and anxiety, with more sleep loss and other sleep disorders.[35][37][38]
Sleep remediation is often employed to alleviate the pain in migraine episodes, and sleep deprivation could also trigger headaches and migraines. Subjects with tension-type headaches, and subjects without were both susceptible to frontal headache due to insufficient sleep. The frequency, duration and intensity of migraines and headaches is perpetuated by sleep deficiency. [35][36] Similarly, patients with chronic migraines are more likely to suffer from Insomnia and other sleep-disordered complications than those with episodic migraines.[38]
Migraine therapies such as Amitriptyline and Propranolol have been found to be incident with yvarious NREM Parasomnias in the course of treatment.[36]
Some sleep disorders are linked with headaches and migraines. These are indicated in the ICSD – International Classification of Sleep Disorders by the AASM – American Academy of Sleep Medicine as:
Migraines:[41] [43]
- Bruxism (Nocturnal Teeth Grinding)
- Insomnia
- Parasomnia (Night Terrors)
- PLMS (Periodic Limb Movement Syndrome)
- RLS (Restless Leg Syndrome)
- Somnambulism (Sleep Walking)
- Somniloquy (Sleep Talking)
- Obstructive Sleep Apnea Syndrome (OSAS)
Cluster Headache:[40]
- Wakefulness, Insufficient Sleep
- Disordered Sleep
- (OSAS) Obstructive Sleep Apnea Syndrome
- (CSA) Central Sleep Apnea
Tension-Type Headache (TTH):[45]
- Insomnia
- Poor sleep quality
Chronic Persistent Headache (Migraine):[43]
- Insomnia
- (OSAS) Obstructive Sleep Apnea Syndrome
Hypnic Headache syndrome (‘Alarm Clock’ Headache):
- ` Nocturnal Awakenings (frequency and duration)
Headache due to head trauma, neck trauma, head injury, neck injury:
- Sleep Disruption
- Nocturnal Awakenings (frequency and duration)
- Delayed Sleep Onset
High-altitude headache (Acute Mountain Sickness – AMS):
- Sleep Disturbances
Morning Headache:
- Sleep Impairment
- Early Awakenings
- Sleep Apnoea
- OSAS – Obstructive Sleep Apnoea (and other sleep-disordered respiratory problems)
- Periodic Leg Movement Syndrome (PLMS)
Primary cough headache:
- Sleep disorders
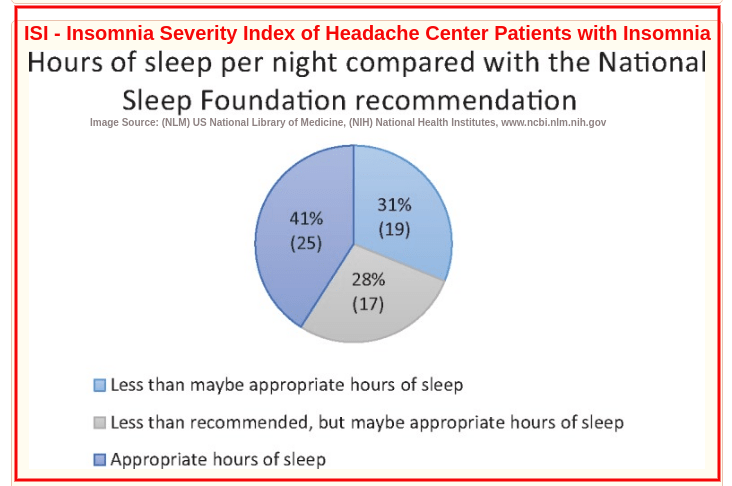
About 50% of patients with chronic headache suffer from self-reported Insomnia with approximately 49% tested positive for clinical Insomnia. Only about 40% have the sleep duration (sleep hours) recommended by the NSF – National Sleep Foundation (i.e. 6-7 sleeping hours for adults). More than 25% of chronic migraine sufferers have an SOL – Sleep Onset Latency of at least 2 hours.[38][42] Migraneurs reported of these sleep problems experienced interictically (episodes in between seizures):[43]
- Difficulty initiating sleep,
- Difficulty staying sleep,
- Poor sleep quality
- Decreased total sleep time
- Excessive daytime sleepiness
- Unrefreshing sleep
A higher predisposal to poor sleep quality and sleep apnea is registered in Chronic Migraine (CM) patients compared to Episodic Migrane (EM,) patients, as was shown in a CaMEO (Chronic Migraine Epidemiology & Outcomes) study. Diagnostic criterion for EM is less than 15 headache days per month, and for CM is 15 or more headache days per month.[44]
The effect of severe tension headaches and migraines and their influence on sleep quality is undisputed, even in paediatric cases.[39] Migraine affects about 10% of school-going children and 28% of teens aged 15-19 years. Studies have shown that children with and due to migraine and its complications,experienced:
- Increased sleep loss (short sleep duration)
- Lower sleep quality (during the headache episode)
Covid-19 Update: Comorbidities
OSAS (Obstructive Sleep Apnea Syndrome) is also indicated as a higher risk factor (8 times more) in Covid-19 infection[46], compared to the same demographic hospitalized in a public health system, and with a much worse effect. The prevalence of respiratory failure in Covid-19 patients with comorbid OSAS was twice as much.
Contraindicated in this are patients with OSAS comorbidites such as:
- Atrial Fibrillation
- Hypertension
- Congestive Heart Failure
- Coronary Artery Disease
- Diabetes
- Stroke
- Mood Disorder
- Cognitive Dysfunction
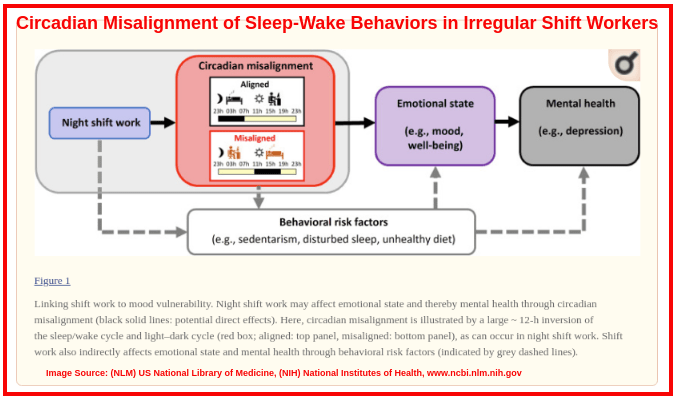
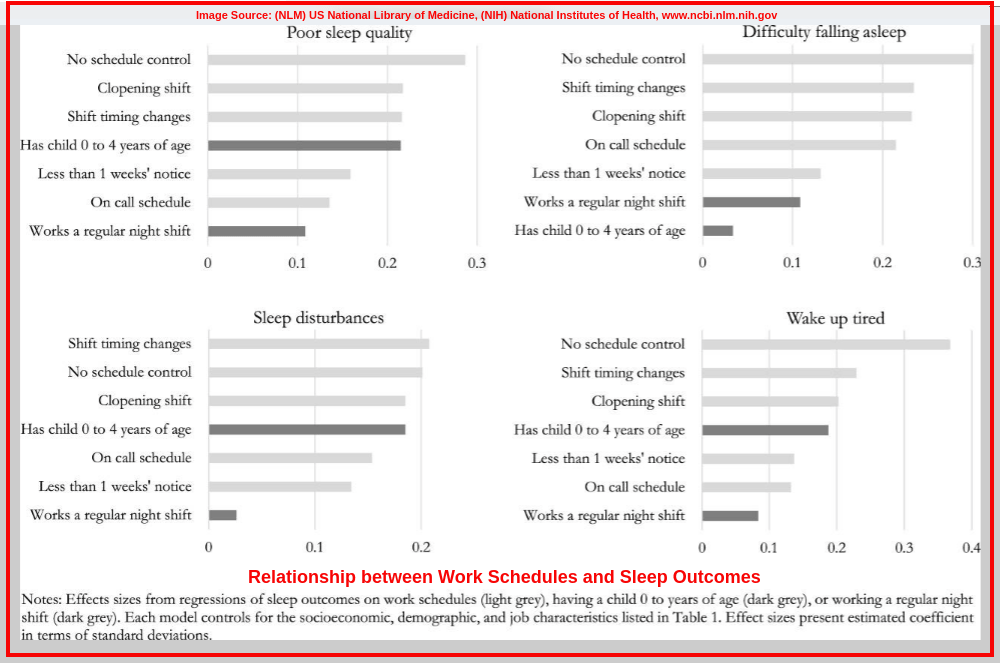
4. Shift Working and Circadian Rhythm
More than 23 million Americans (about 16% of wage and salary workers) do shift work. Of these, about 6% work evening shifts, another 4% work night shifts, and the others work irregular shifts (rotation shifts, split shifts). About 9.2 million (40%) of these shiftworkers do so because of the nature of the job; approximately 3 million (12%) do the shift-work as a part-tme job; and another 4.3 million (19%) are shiftworking as a personal preference.[47]

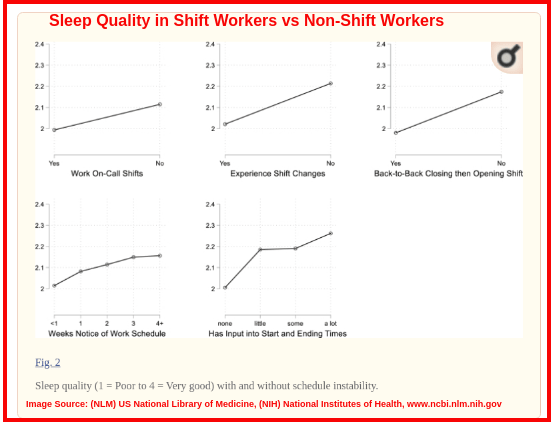
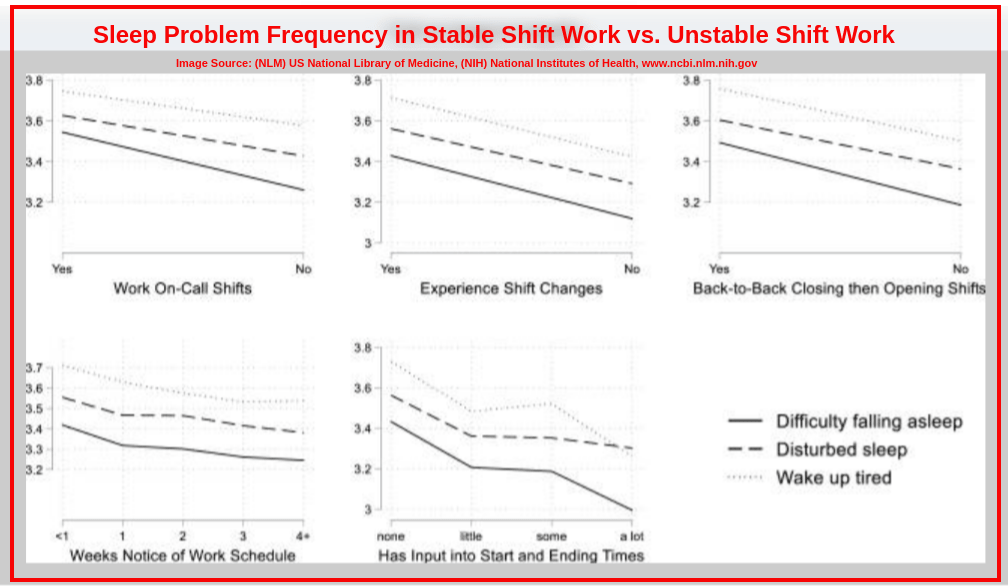
Sleep Contraindication: Shift Working, Circadian Rhythm
Central to the Circadian Rhythm, work schedules,life patterns and routines is time. The “non-standard working hours” entail: work hours in the weekends, night shifts, evening shifts, early morning shifts, continuous closing and opening “clopening shifts”; and also include: on-call work shifts, last minute scheduling work shifts, just-in-time work schedules, short notice work shifts. They are imminent in the American economy and are associated with:[48][49][50][51][52]
- disrupting circadian cycles
- dysregulated sleep patterns
- misaligned sleep-wake behaviours
- negatively impact sleep quality
- shorter sleep duration (less than 6 hours)
- excessive daytime sleepiness – up to 95% of irregular shift workers
- stress
- mood disorders (irritability, anxiety)
- psychological distress
- cognitive dysfunction
- poor mental health (self-rated)
- worsening health and overall well-being (self-rated)
- “role blurring” – taking work to home for work extension (working after hours at home)
- risk of burnout – up to 95% of irregular shift workers
- higher Emotional Exhaustion (EE) – more than 23% – 95% of irregular shift workers
- lower perceived lack of Personal Achievement (PA) – more than 40% of irregular shift workers
- higher Depersonalization (DP) – more than 42% – 95% of irregular shift workers
- weight problems, high BMI (overweight, obese)
5. Sedentary, Inactive Lifestyle vs. Physical Activity
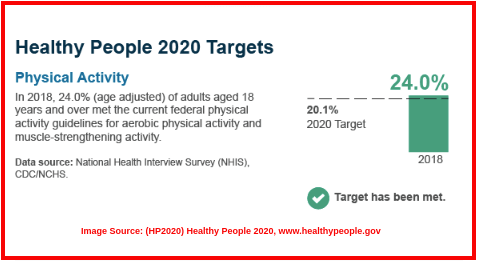
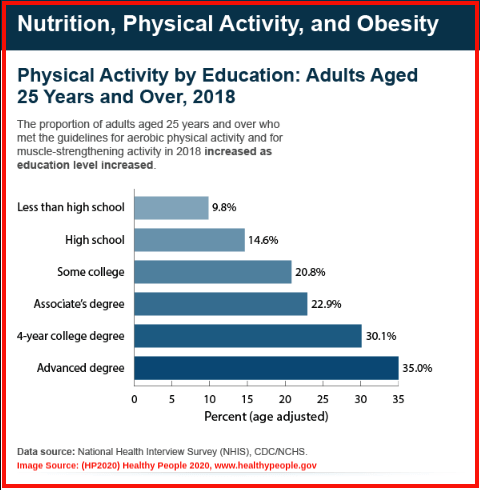
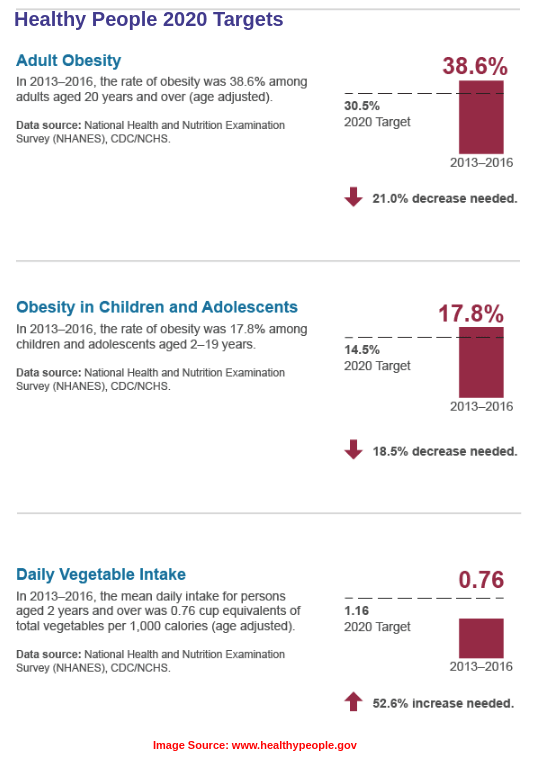
By year 2019, only 1 in 4 American adults and 1 in 5 adolescents in the US met the standard health guidelines for physical activity (which includes aerobic exercise and muscle training). Utah stands at 18.5% as the healthiest state with Mississipi being the least healthiest state (37.7%)according to CDC data on metrics of physical inacivity. These are persons who registered no physical activities other than those engaged in at their workplaces in the past month. Nonetheless, the HP2020 – Healthy People 2020 targets were attained for physical activity in 20.1% of adults aged 18 years and above.
Sleep Contraindication: Sedentary, Inactive Lifestyle, vs. Physical Activity
There is a proven relation between the physiological mechanisms through which one’s health is affected by Sleep or Sleeping and:[56][57][58][59]
- SB (Sedentary Behavior) – includes activities such as talking, sitting at an office desk or at a table, eating, riding as a passenger, driving, watching television.
- LIPA (Light-Intensive Physical Activities) – other activities that are not classified as Sleep, SB or MVPA; including: house chores, cleaning, cooking, light gardening, standing, shopping, walking.
- (MVPA) Moderate-to-Vigorous Physical Activity – includes activities such as swimming, cycling, jogging, exercising, Also classified as:
- Moderate Physical Activity (MOD-PA),
- Vigorous Physical Activity (VIG-PA).
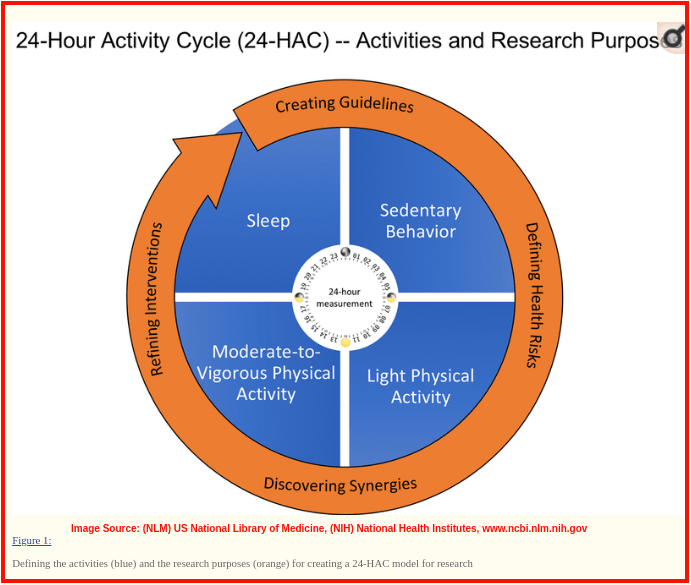
Metabolic Equivalent of Task (MET) Hours: used to express energy expended in a physical activity. 1 MET is equivalent to energy expended when seated at rest.
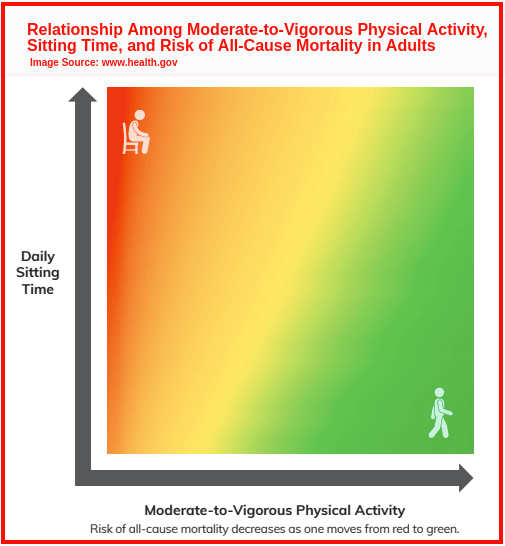
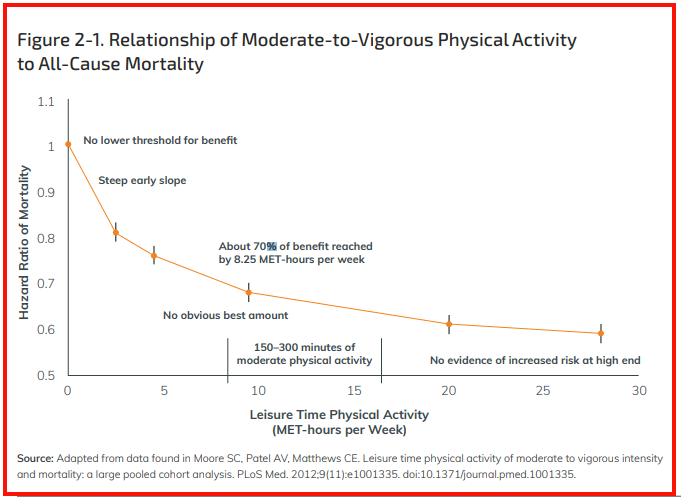
Studies have shown the great benefits in cardiac and metabolic health realized from increased time in Moderate-to-Vigorous Physical Activity (MVPA). It is associated with:[56][57][58][59]
- shorter sleep onset latency, SOL (ease of falling asleep)
- Improved sleep efficiency (deeper sleep)
- improved perceived sleep quality
- better wakefulness (morning alertness)
- reduced sleepiness
MVPA, LIPA, MOD-PA and VIG-PA are associated with:[56][57][58][59]
- decreased odds of Insomnia
High amounts of MVPA (Moderate-to-Vigorous Physical Activity) that’s >0 and
- decreased odds of long sleep duration
- shorter sleep duration
- decreased odds of aveerage sleep quality
- increased odds of better sleep quality
- increased odds of higher sleep efficiency
- decreased odds of restless sleep, non-restorative sleep (for MVPA that’s >11.25 MET-hourr/week)
* * The greatest beneficiaries of better sleep quality through higher MVPA are older persons and individuals with poorer sleep quality. * *
Light Physical Activity (LIPA) of >0 MET-hours/week is associated with:[56][57][58][59]
- decreased odds of short sleep duration
Higher amounts of Total Physical Activity, LIPA and MOD-PA are associated with:[56][57][58][59]
- decreased odds of poor sleep quality
Higher SB, Sedentary Behavior time of >11 hours/day is associated with:[56][57][58][59]
- increased odds of short sleep duration
- decreased odds of early sleep onset (delayed sleep)
- increased odds poor sleep quality
- increased odds of Insomnia symptoms
- increased odds of Obstructive Sleep Apnea Syndrome (OSAS )
6. Diet
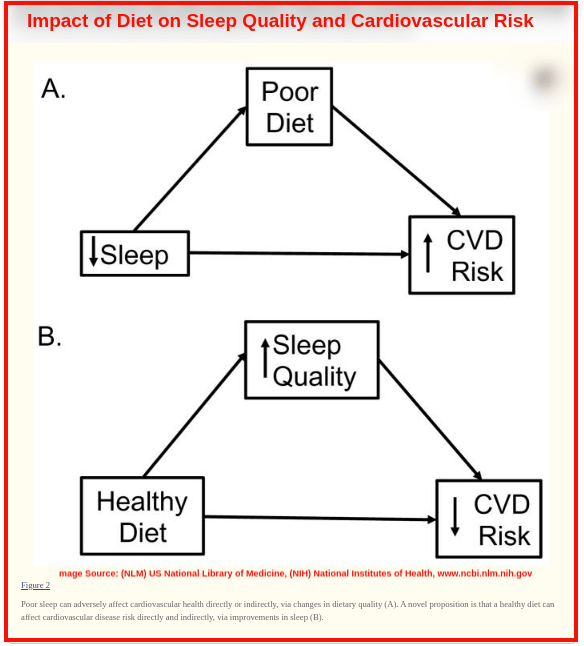
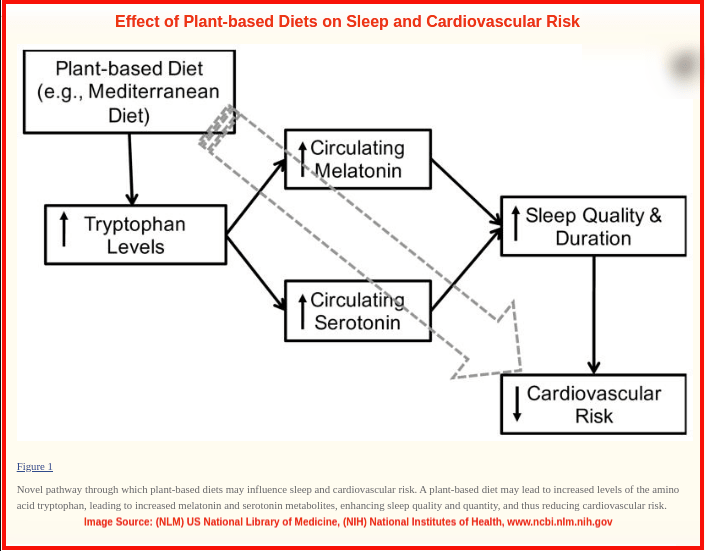
The digestion and absorption of food intake is involved in the processes of sleep regulation, which include metabolism and cardiac mechanisms. Diet also determines fitness and health levels, while also playing a major role in immunity. Improving diet through superfoods full of nutrition can help regulate the body better, helping with restful sleep as well. Key dietary pointers that influence sleep and have been scientifically shown to improve sleep quality include:[60][61][62][63]
Sleep Contraindication: Diet
Tryptophans
Tryptophans are essential amino acids that are synthesized in the body in production of the sleep hormones, Melatonin (regulation of the Circadian Rhythm, sleep-wake cycle)and Serotonin (sleep modulation, precursor of Melatonin).[60][62]
Tryptophan-rich foods have been shown to impact sleep aspects as follows:[60][62]
- increased Total Sleep Time (TST) = Total REM sleep time + Total NREM sleep time
- Increased sleep efficiency
- increased ease in falling asleep, sleep onset latency (SOL)
- decreased nocturnal awakenings
- decreased sleep fragmentation
Dietary Tryptophan is obtained from: whole milk, cheese eggs (egg-white), nuts, seeds, oats, cereals, tuna fish, chicken, turkey. Plant-based Tryptophan sources are just as beneficial for better sleep quality and in sleep quantity as the animal-based Tryptophan sources.[60][62]
Depletion of dietary Tryptophan in the body disrupts Serotonin synthesis and function, thereby causing:[60][62]
- reduced sleep quality
- induced sleep impairment
- decreased REM sleep onset latency (SOL)
Isoflavones
Isoflavones are found in plant-based proteins which give the plant pigmentation. They are, anticancer, anti-inflammatory, antimicrobial, antioxidant, and sleep promoting properties beneficial in improved sleep quality.[62] Sources rich in isoflavones are mainly legumes, and include: soybeans, peanuts, chickpeas, beans, nuts and fruits.
They influence sleep outcomes by:
- reduced sleep duration
- increasing sleep quality
- reduced daytime sleepiness (especially in women, due to the estrogenic properties of Isoflavones)
Macronutrients
Diet with high Glycemic Index (GI) influences sleep by:[60]
- shortened sleep onset latency (SOL) – when taken 4 hours before to bedtime
Diet with high Carbohydrate content influences sleep by:[60]
- shortened sleep onset latency (SOL) – when taken 4 hours before to bedtime
- increased sleep arousals
Diet with very low Carbohydrate content impacts sleep by:[60]
- increased sleep arousal index of the NREM 1 (N1 sleep) and NREM 2 (N2 sleep)
- increased TST – total sleep time of the combined NREM 1 – NREM 4 (N1, N2, N3, and N4 sleep)
- reduced ratio of REM sleep time to total sleep time (TST)
Diet with high Fiber intake influences sleep by:[60][62]
- reduced NREM 1 (N1 sleep)
- increased NREM 3 (N3 sleep)
- increased SWS (slow wave sleep) duration
Diet with high Protein influences sleep by:[60]
- improved sleep quality
- reduced daytime sleepiness
- reduced sleep intervention and napping
- reduced awakenings
Diet with high Fat content influences sleep by:[60][62]
- increased sleep onset latency (SOL)
- reduced sleep quality
- reduced NREM 3 (N3 sleep)
- Reduced SWS (slow wave sleep) duration
Diet with high Sugar intake influences sleep by:[60][62]
- increased sleep arousals
- increased nocturnal awakenings
The consensus based on data from scientific research indicates that sleep quality and sleep quantity invariably benefit from dietary patterns with:[60][62]
- high complex carbohydrates
- low saturated fats (e.g. plant-based diets)
- high fiber content
Food Items
Cherries: rich in phytonutrients such as Serotonin, Melatonin, sleep hormones, aid in:[60]
- improved sleep duration
- Improved sleep quality
- increased Total Sleep Time (TST) (in elderly, middle-aged and young age groups)
- increased sleep efficiency (in elderly age groups)
- reduced nocturnal awakenings (in elderly, middle-aged and young age groups)
- reduced nocturnal activity (in elderly, middle-aged and young age groups)
- decreased SOL sleep onset latency (in elderly, middle-aged and young age groups)
- reduced daytime sleepiness and napping for sleep loss intervention
Seafood (Oysters, Krill): rich in minerals such as Zinc, and aid in:[60]
- improved sleep quality
- improved sleep onset latency (SOL)
- increased sleep efficiency
- increased Total Sleep Time (TST)
- decreased nocturnal awakenings
Dietary Habits
Americans are guilty as charged on various counts of dietary habits that are detrimental to good sleep outcomes, and these include:[60][61][63]
- skipping Breakfast – which causes inadequate sleep(reduced sleep sufficiency); and Circadian entrainment (enhanced regulation of the sleep-wake cycle) [60][61]
- eating Fast Foods – which causes low sleep quantity (reduced TST, total sleep time)
- excessive Sweets – which causes poor sleep (reduced sleep quantity); and increases sleep arousals (increased nocturnal awakenings)[60][61]
- unscheduled Feeding and unregulated Meal-timing – which causes sleep-wake dysregulation (disrupted Circadian clocking)[60][61]

7. Age
Senior citizens in America, aged 60 years and above, accounted for about 16.5% (about 52.7 million) of the US population in year 2019. They were more than 51 million in year 2018, going by Census 2019 data from the United States Census Bureau.[64]
Statistical data from the National Sleep Foundation (NSF) revealed that at least 53% of Americans of old age without any chronic conditions had sleep problems, and more than 80% of elderly Americans with 4 or more chronic conditions also had sleep dysfunction.[65]
Sleep Contraindications: Age
Aging and changes in sleeping patterns coincide with the progression of time, and such changes include:[65]
- diagnoses of about 5% with Insomnia
- diagnoses of about 20% with Sleep Apnea syndromes
- incremental aggregation of Obstructive Sleep Apneas and Hypopneas (OSA, OSH)
- general diminished sleep quality
- increased sleep fragmentation
- aggravated daytime sleepiness
- increased incidences of Narcolepsy
- increased sleep inadequacy and sleep loss
- diagnoses of SBD, Sleep-Disordered Breathing
- increased incidences of sleep dysregulation
Further, age-related cognitive and neuronal degeneration and dysfunction has a direct association with sleep function, including, the expression and mutation of sleep regulatory genes such as:[65][70]
- BMAL1 (Brain and Muscle Arnt-Like 1) – linked in sleep loss and sleep insufficiency; peaks in the morning Wake-Cycle.
- CLOCK (Circadian Locomotor Output Kycles Kaput) – linked in Circadian biorhythms and in Insomnia; peaks in the morning Wake-Cycle.
- CRY (Crystal) – linked in sleep homeostasis; peaks at night in the Sleep-Cycle
- PER (Period) – for alertness in the Sleep-Wake Cycle, and sleep homeostasis; peaks at night in he Sleep-Cycle
Lost or repressed expression of the rhythmic cycling of these Circadian clock genes, is often attributed to neurodegenerative conditions like Alzheimer’s and Mild Cognitive Impairment, and could result in:[65][70]
- Circadian Rhythm dysfunction (Sleep-Wake Cycle dysregulation)
- diminished sleep quality
- diminished sleep consolidation (to equate total time in bed – TIB, with total sleep time – TST)
- increased sleep debt
- increased daytime sleepiness
The regressive sleep outcomes in sleep quality and sleep quantity are interlinked in a vicious cycle with other age-related degenerative diseases and conditions, which include: Dementia, Alzheimer’s Disease (AD), Subjective Cognitive Decline (SCD) and Mild Cognitive Impairment (MCI).[65][69]
● Dementia
Dementia has been associated with various sleep outcomes:[65]
- increased daytime sleepiness (also used as a predictive symptom of Dementia)
- Increased sleep insufficiency
- diminished sleep quality
- prolonged sleep time (used in indicating Dementia)
- increased risk of SDB, Sleep Disordered Breathing
- increased risk of RBD, Rapid Eye Movement Sleep (REM) Behavior Disorder (in Dementia with Lewy Bodies, DLB)
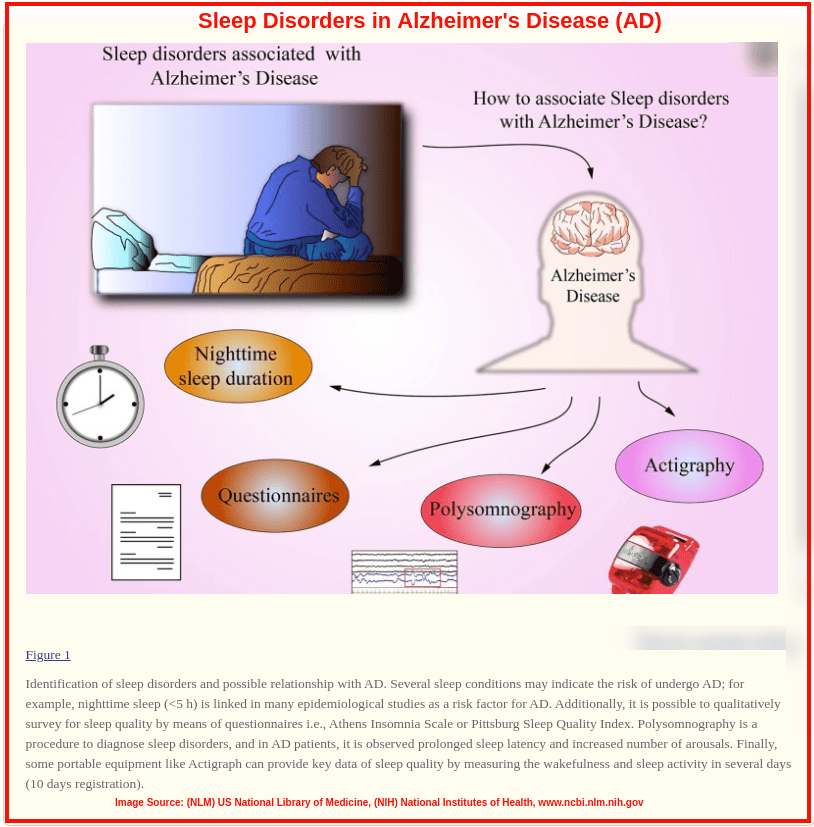
● AD – Alzherimer’s Disease
About 60% of individuals with AD also suffer from correlated sleep problems.Alzheimer’s Disease is linked to the following sleep problems:[65][69]
- increased sleep fragmentation
- increased SWS slow wave sleep activity
- increased risk of SDB, Sleep Disordered Breathing
- increased risk of Insomnia
● SCD – Subjective Cognitive Decline, MCI – Mild Cognitive Impairment
MCI, Mild Cognitive Impairment is often indicative Alzheimer’s Disease, diagnosed by under par performance in neurological and psychological testing. Self-assessed memory impairment may also present itself prior to the clinical manifestation of MCI, which is diagnosed as SCD, Subjective Cognitive Decline.[65][66][67][69]
The counteractive interrelation between “subjective” cognitive dysfunction and sleep impairments further elicits the folowing sleep outcomes in MCI and SCD, whereby just about as many MCI patients as Alzheimer’s patients with sleep disruption.[65][66][68][69]
- sleep loss due to severe SCD
- low sleep quality
- reduced sleep efficiency
- daytime sleepiness and daytime dysfunction
- reduced sleep latency (due to sleep debt)
- reduced sleep time
- high scores on the Pittsburgh Sleep Quality Index (indicating decreased quality of sleep, sleep disturbance)
- increased incidences of sleep disorders
Age-related atrophying of gray matter in the pre-frontal cortex of elderly individuals causes:[65]
- reduced NREM sleep (Non-Rapid Eye Movement)
- reduced SWS (slow wave sleep) activity
- impaired cognitive function and memory retention that’s sleep-dependent
- reduced total sleep time (sleep duration)
- increased (self-reported) daytime sleepiness
Age-related thinning of the cortical superior frontal lobe, and age-related volume changes of the Hippocampus are linked in:
- (gender-specific, female prevalent) Obstructive Sleep Apnea
- increased (self-reported) daytime sleepiness
Thinning of the lower left Entorhinal cortex which progresses with age is linked in:
- shorter sleep duration (reduced TST, total sleep time)
8. Stress
Any tension that disrupts one’s mental, emotional, psychological, or physical well-being is termed as “stress”; while any factors causing such physiological and psychological tension (stress) are termed as “stressors”. In tandem is the severity of manifested physical or mental tension resulting from factors that alter an existing equilibrium, which is termed as the “stress level”(in the NOC, Nursing Outcomes Classifications).
Stress, Stressed, Stressors in America
The “Stress in AmericaTM” 2020[70] survey revealed that Americans are dealing with unprecedented levels of immense stressors, in this COVID-19 era. With more deaths in the US (500,000+) than the combination of those recorded in World War 1, the Korean War, andthe Vietnam War, Americans (and the world over) are experiencing the most stressful grievous crisis. In what is an full arsenal of very real and relevant stress factors, the numbers show that:[70]
- About 78%, every 8 in 10 adults in the US consider the COVID-19 pandemic to be a major stressor in their lives
- About 67%, every 2 in 3 American adult have experienced increased stress levels since the beginning of the COVID-19 pandemic
- About 49%, every 1 in 2 US citizens, has had a negative behavioral change from the increased stressors in the COVID-19 period, affecting them physically, emotionally and mentally (including, temper tantrums, anxiety and mood swings)
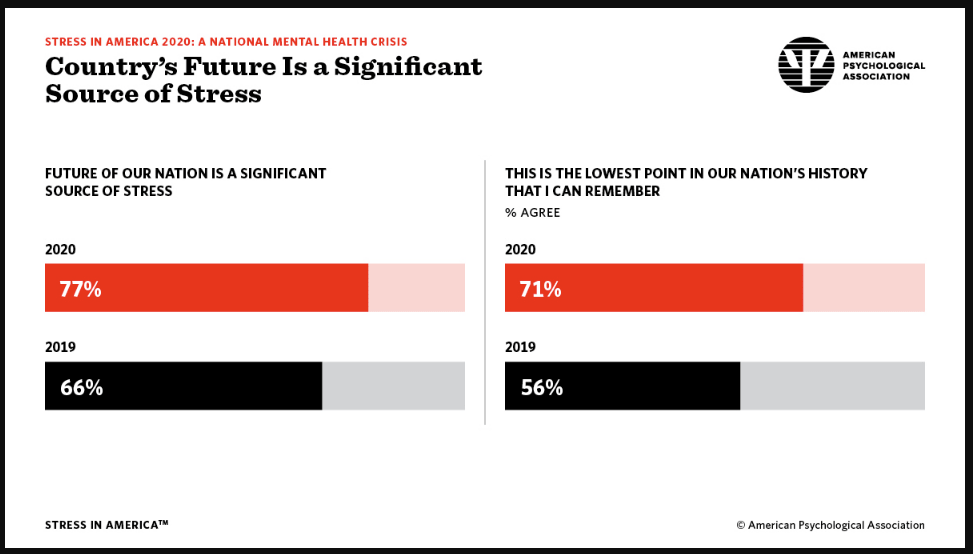
- About 77%, every 3 in 4 Americans, is stressed about the future of the nation in year 2020, when the same stress factor was indicated by about 66% in year 2019

Other stress factors Americans stated in the survey include:[70]
- Global Warming and Climate Change (about 55%)
- Gun Violence (more than 60%)
- Healthcare (about 70%)
- Immigration (about 47%)
- Opioid crisis (45%)
- Sexual harassment and sexual assault (almost 50%)
- Suicidality (more than 50%)
Sleep Contraindication: Stress
Sleep Reactivity vs. Stress Reactivity
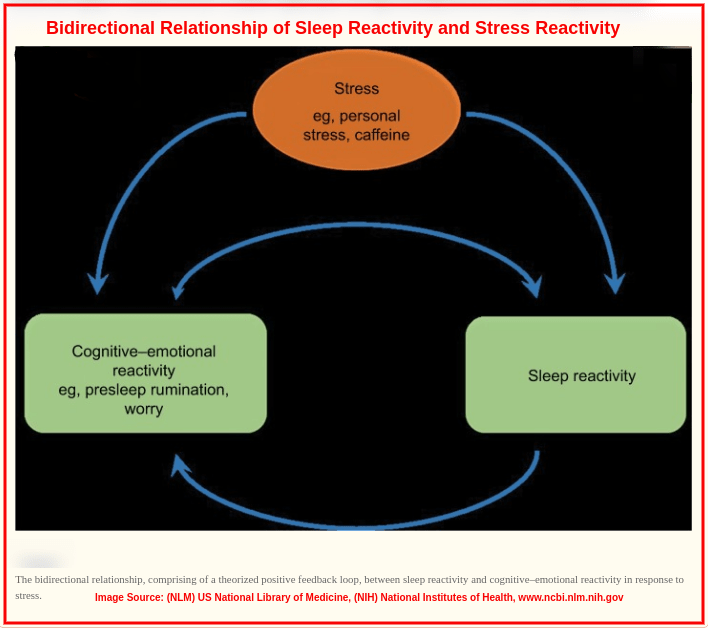
Stress and sleep have a bidirectional relationship whereby exposure to stress causes these sleep complications (depending on individual sleep reactivity and the preceding stress reactivity)[71]:
- difficulty initiating sleep
- difficulty maintaining sleep
- HPA disruption (sleep disturbance)
To combat the consequences of sleep and stress reactivity, many often consume medications like anti-depressants. However, a section of the population often relies on CBD products like edibles and tropicals, which can be delivered by Healing Nug Delivery (known to be a reputed long beach weed delivery firm).

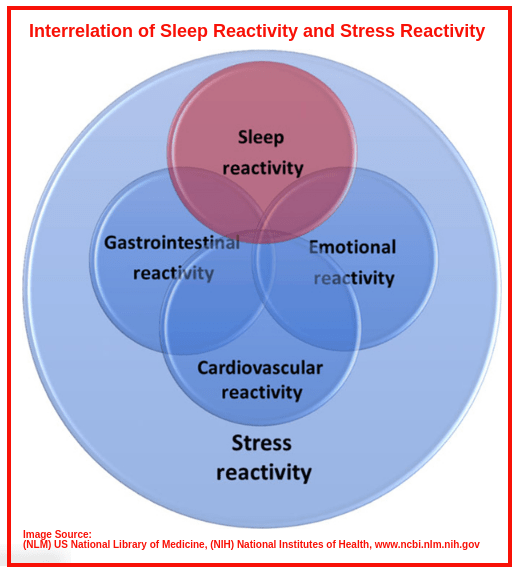
Stress Reactivity:
The physiological and psychological response to stress, stressors and stress levels with a component of sleep disturbance is defined as Stress Reactivity.[71][72] It is also referred to as: “sleep sensitivity”, “sleep system sensitization/sensitivity” or sleep hypersensitivity.
Studies have shown that stress reactivity negatively impacts the sleep profile with:[71][72]
- sleep reactivity
- situational insomnia
- hyperarousal
Stress arises from, among other issues, material hardship which stimulates psychological distress and physiological hindrances to sleep. It is further shown to cause the following sleep outcomes in affected persons from the Michigan Recession and Recovery Study:[73][71][72]
- increased sleeplessness
- reduced sleep quality
- increased sleep insufficiency
- increased daytime sleepiness
- prolonged sleep onset
- increased sleep hyperarousal (bedtime agitation)
- reduced sleep duration (less than optimal total sleep time)
Sleep Reactivity:
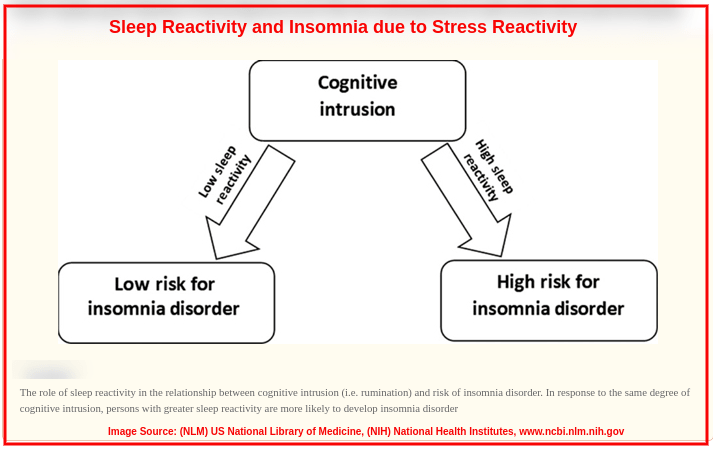
The degree by which exposure to stress causes sleep disruption is referred to as Sleep Reactivity.[71][72] It modulates the impact of stress on sleep physiology.
Research reveals that sleep reactivity is influenced by: environmental stress, genetics, gender, familial Insomnia,
There is a bidirectional relationship between sleep reactivity and stress reactivity.
People with high sleep reactivity have been scientifically shown to exhibit the following sleep changes in their sleep profile:[71][72]
- increased incidence and chronicity of Insomnia (short sleep Insomnia, sleep onset Insomnia)
- iIncreased sleep latency, (in Insomnia-free cases responding to stress),which was comparably similar to the sleep onset latency of insomniacs
- difficulty initiating sleep
- difficulty maintaining sleep
- reduced REM sleep duration (short REM sleep, fragmented REM sleep)
- increased sleep arousals
- increased nocturnal awakenings
It has been proven that there is no difference in the sleep profiles of unstressed sleepers with high sleep reactivity and of unstressed sleepers with low sleep reactivity.[71][72]

9. Fatigue and Burnout
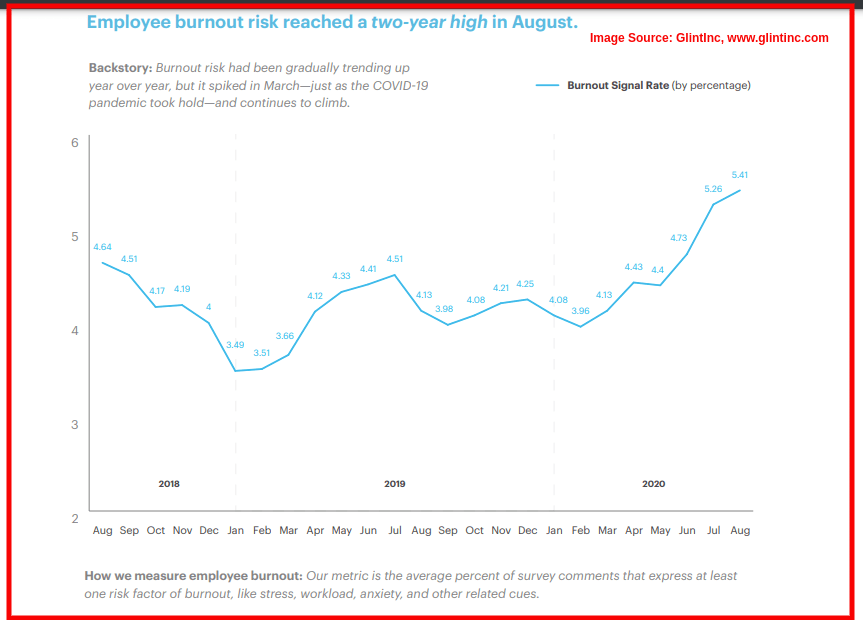
By the year 2020, the Burnout numbers among polled employees had reached a 2-year high at 5.41% in August, compared to 4.13% in August-2019, and 4.64% in August-2018. The spike in March of 2020 was owed to the Covid-19 pandemic which further complicated employee performance.
Fatigue
“Fatigue” is defined as the physiological reduction in muscle and/or organ efficiency after engaging in prolonged activity. Fatigue is characterized by:
- excessive tiredness
- low energy levels
- reduced efficiency
- disruption in normal activities or work
- sleepiness or increased need for sleep
Burnout
“Burnout” is defined as a state of compromised health due to overworking, chronic job stress (excessive, prolonged stress), and complete exhaustion. Burnout is characterized by:
- Psychological manifestations:
- feeling overwhelmed
- feeling emotionally drained
- increased self-doubt
- increased sense of underachievement
- increased sense of helplessness, defeat
- feeling trapped
- lack of motivation
- increased negativity and cynicism
- decreased effectiveness and efficiency
- decreased sense of satisfaction
- Depression and Anxiety[74][75]
- Physical manifestations:
- Ineffectiveness and inefficiency
- reduced throughput and work output
- underperformance and underachievement
- incomplete tasks, unfihished projects
- Sleep Disorders[74][75]
Sleep Contraindication: Fatigue and Burnout
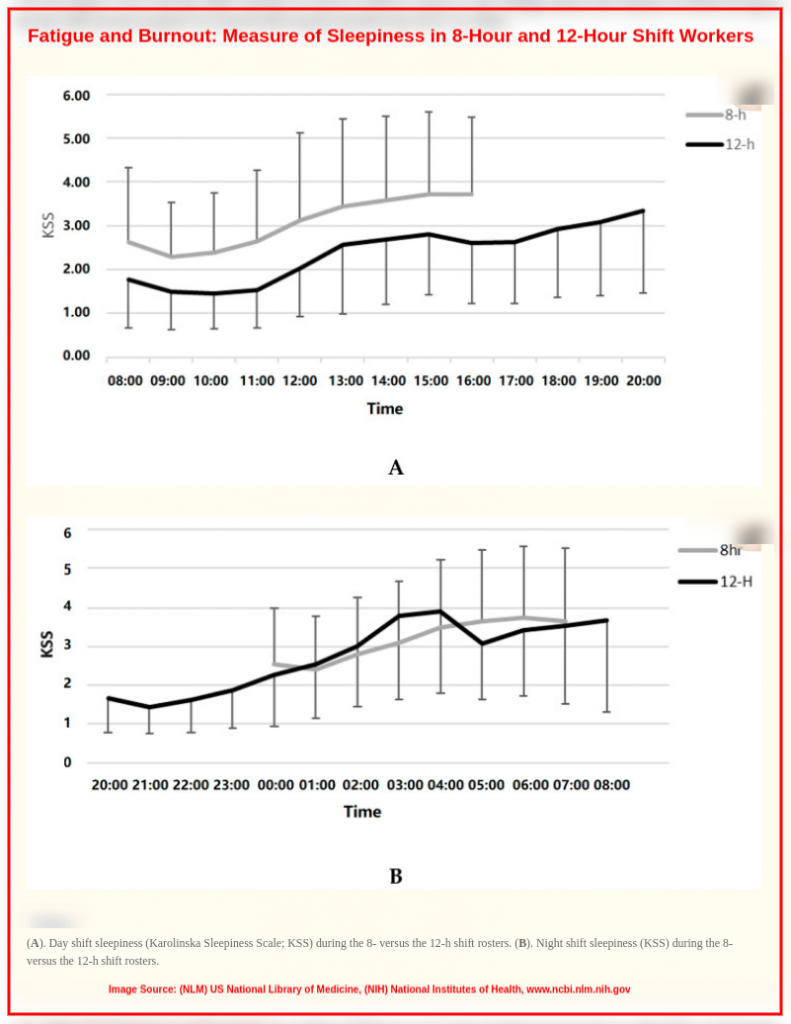
Numerous studies on employees working full-time in 8-hour and 12-hour shifts have analyzed the following sleep outcomes in the workers as pertaining to fatigue and burnout:[74][75][75]
- increased sleep debt (arising from reduced sleep duration)
- diminished sleep quality
- diminished sleep efficiency
- increased sleep loss and sleep deprivation
- increased daytime sleepiness and nappiness
The sleep outcomes associated with fatigue and burnout are bidirectionally linked in a vicious cycle, where primary sleep problems further aggravate the fatigue and burnout symptoms, and secondary sleep disruption is realized.[74][75][75]
Fatigue and Burnout alter metabolism which then causes:
- Circadian Rhythm disruption
- Sleep-Wake cycle disorders (Hypersomnias and Insomnias, RBD – REM sleep Behaviour Disorder)
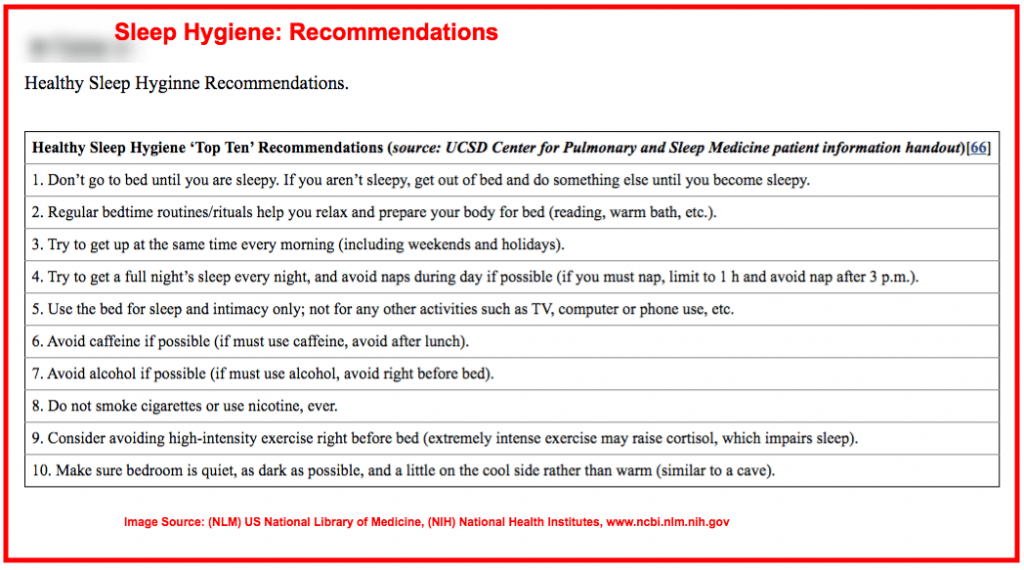
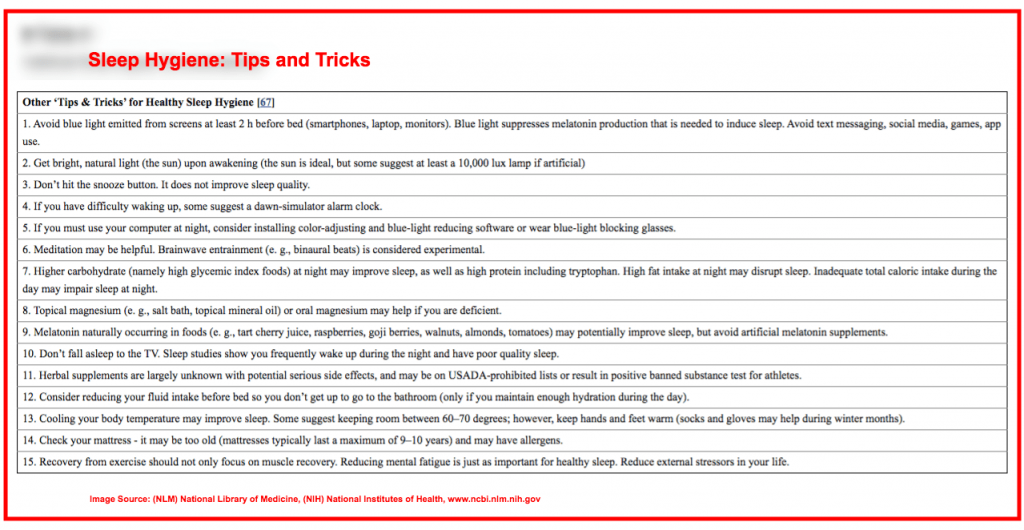
10. Sleep Hygiene
Sleep experts have defined Sleep Hygiene as both:
- the practising of habits that promote healthy sleep, giving better sleep quality, and,
- the avoidance of habits that cause sleep disruption and give low sleep quality.
Sleep Hygiene is negatively impacted by the following practices and situations:
Schedules:-
- irregular schedules for mealtimes
- inconsistent sleep schedules
Diet:-
- insufficient regular intake of vegetables
- excessive daily consumption of caffeine
- taking meals before bedtime
Sleeping Area:-
- lack of sunlight in the morning in the bedroom
- using electronic screens and displays in bed
Before-Sleep Habits:-
- poor sleep-related cognition
- bad attitudes towards sleep
- poor emotions at bedtime
Sleep Habits:-
- nocturnal awakenings
After-Sleep Habits:-
- skipping daily breakfast meals
- lack of morning sunlight exposure

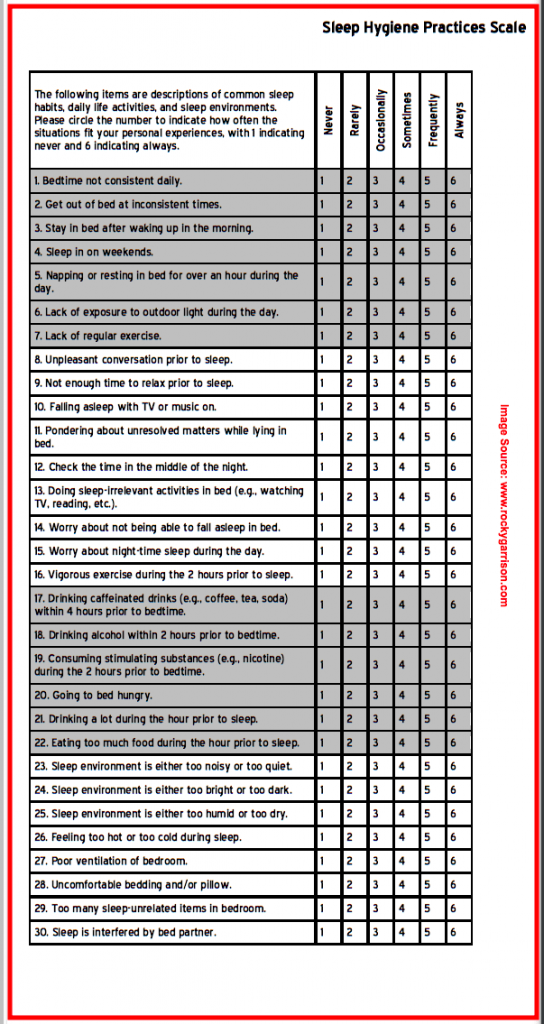
The SHPS – Sleep Hygiene Practice Scale is used to evaluate the awareness and practice of good sleep hygiene practices, using several key pointers as listed below.
Sleep Contraindication: Sleep Hygiene
Research studies have revealed effects of the following sleep hygiene don’ts:
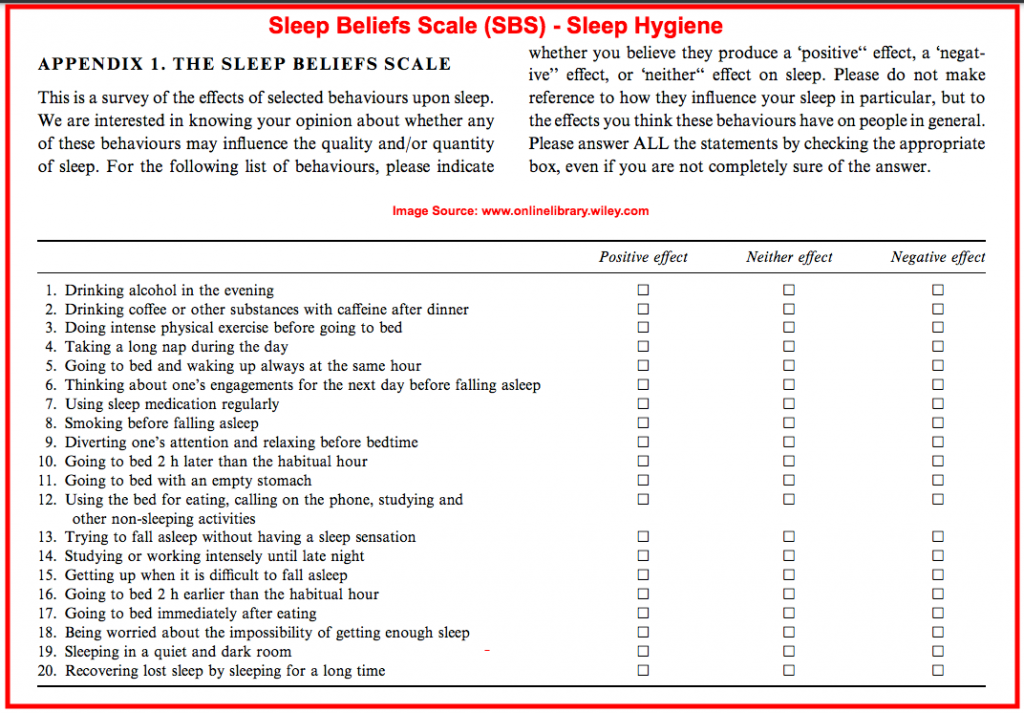
- Subjects with dysfunctional beliefs about sleep were more likely to report poor sleep quality.[77]
- Subjects who engage in other non-sleep activities (e.g. watching TV, reading a book) during bedtime are more prone to having daytime somnolence, with increased nappiness (need for taking naps).[77]
- Subjects living in neighborhoods lacking social cohesion and support, with violence and high crime rates, with excessive noise and light have a higher risk of:[77]
- daytime sleepiness
- short sleep duration
- non-restorative sleep
- sleep insufficiency (sleep debt)
- low sleep quality
- sleeping disorders
- Elite athletes have registered much less total sleep time (TST), and reduced sleep efficiency than non-athletes. They experience reduced wakefulness and alertness in the Wake-cycle, together with (sleep hormone) Melatonin disruption, which causes Circadian Rhythm dysregulation due to:[78]
- overuse of smartphones and other electronic gadgets at bedtime (sleep hygiene malpractices)
- prolonged exposure to glaring screens and blue light at bedtime (unhealthy sleep hygiene)
Highlighted below are the sleep hygiene do’s and don’ts for a healthy sleep profile.
REFERENCES:
< Introduction >
[1] NHLBI (National Heart, Lung, and Blood Institute). National Sleep Disorders Research Plan, 2003. Bethesda, MD: National Institutes of Health; (2003). https://www.ncbi.nlm.nih.gov/books/NBK19961/
[1] Sleep Problems, Comorbid Mental Disorders, and Role Functioning in the National Comorbidity Survey Replication (NCS-R)
[2] Insufficient Sleep in the United States, 2020 Annual Report; AHR – America’s Health Rankings. (2018) https://www.americashealthrankings.org/explore/annual/measure/sleep/state/ALL
< 1. Medication >
[3] Prescription Drug Use in the United States, 2015–2016; NCHS Data Brief No. 334, May (2019) https://www.cdc.gov/nchs/products/databriefs/db334.htm
[4] Medicine Use and Spending in the U.S. A Review of 2018 and Outlook to 2023. IQVIA Institute Report, May 09, (2019). https://www.iqvia.com/insights/the-iqvia-institute/reports/medicine-use-and-spending-in-the-us-a-review-of-2018-and-outlook-to-2023
[4] Nearly One in Two Americans Takes Prescription Drugs: Survey (2019) https://www.bloomberg.com/news/articles/2019-05-08/nearly-one-in-two-americans-takes-prescription-drugs-survey
[5] Prevalence of Prescription Pain Medication Use Among Adults: United States, 2015–2018; NCHS Data Brief No. 369, June (2020) https://www.cdc.gov/nchs/products/databriefs/db369.htm
< Chronic Pain >
[6] Prevalence of Chronic Pain and High-Impact Chronic Pain Among Adults – United States, 2016 (2018) https://www.cdc.gov/mmwr/volumes/67/wr/mm6736a2.htm
[6] QuickStats: Percentage* of Adults Aged ≥20 Years Who Had Chronic Pain, by Veteran Status and Age Group – National Health Interview Survey, United States, 2019 (2020) https://www.cdc.gov/mmwr/volumes/69/wr/mm6947a6.htm
[7] Chronic pain: a review of its epidemiology and associated factors in population-based studies (2019) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6676152/
[7] Analysis of the effects of a tricyclic antidepressant on secondary sleep disturbance induced by chronic pain in a preclinical model (2020) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7714178/
[7] Chronic exposure to insufficient sleep alters processes of pain habituation and sensitization (2019) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5832516/
[8] The prevalence and awareness of sleep apnea in patients suffering chronic pain: an assessment using the STOP-Bang sleep apnea questionnaire (2018) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6078087/
< NMU and NMUPD >
[9] Association Between Nonmedical Use of Prescription Drugs and Sleep Quality in a Large College Student Sample (2019) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5949251/
[10] Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area (2020) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7177629/
[10] Chronic Pain Management during the Covid-19 Pandemic: A Scoping Review (2020) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7706418/
[11] Self-Esteem and Non-Medical Use of Prescription Drugs among College Students: Coping as a Mediator (2020) https://www.tandfonline.com/doi/full/10.1080/10826084.2020.1735441 https://doi.org/10.1080/10826084.2020.1735441
< 2. Comorbidities >
[12] An Empirical Study of Chronic Diseases in the United States: A Visual Analytics Approach to Public Health (2018) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5876976/
< Mental Illness: Depression, Anxiety >
[13] Symptoms of Depression Among Adults: United States, (2019) https://www.cdc.gov/nchs/products/databriefs/db379.htm
[14] Epidemiology of Adult DSM-5 Major Depressive Disorder and Its Specifiers in the United States (2018) https://jamanetwork.com/journals/jamapsychiatry/fullarticle/2671413
[15] Understanding Problems With Sleep, Sexual Functioning, Energy, and Appetite Among Patients Who Access Transdiagnostic Internet-Delivered Cognitive Behavioral Therapy for Anxiety and Depression: Qualitative Exploratory Study (2020) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7592064/
[16] Comorbid Insomnia and Psychiatric Disorders (2018) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5906087/
[16] Depression in sleep disturbance: A review on a bidirectional relationship, mechanisms and treatment (2019) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6433686/
< Cancer >
[17] Cancer, sleep problems, and mind-body medicine use: Results of the 2017 National Health Interview Survey (2019) https://pubmed.ncbi.nlm.nih.gov/31524958/
[18] Molecular Mechanisms of Cancer-Induced Sleep Disruption (2019) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6600154/
< FM - Fibromyalgia >
[19] The Prevalence and Characteristics of Fibromyalgia in the 2012 National Health Interview Survey https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4575027/
[19] Cognitive behavioral treatments for insomnia and pain in adults with comorbid chronic insomnia and fibromyalgia: clinical outcomes from the SPIN randomized controlled trial (2019) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6424087/
[19] Fibromyalgia, https://www.cdc.gov/arthritis/basics/fibromyalgia.htm
[20] Sleep Discrepancy in Patients With Comorbid Fibromyalgia and Insomnia: Demographic, Behavioral, and Clinical Correlates (2018) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6223568/
[20] Discrepancies in Sleep Diary and Actigraphy Assessments in Adults with Fibromyalgia: Associations with Opioid Dose and Age (2020) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6355390/
[20] Paradoxical insomnia and subjective-objective sleep discrepancy: A review (2018) https://pubmed.ncbi.nlm.nih.gov/29402512/
[20] Subjective-objective sleep discrepancy in patients with insomnia during and after cognitive behavioural therapy: An actigraphy study (2020) https://pubmed.ncbi.nlm.nih.gov/32431047/
< CFS/ME - Chronic Fatigue Syndrome >
[21] Chronic Fatigue Syndrome (2020) https://www.ncbi.nlm.nih.gov/books/NBK557676/
[22] Estimating Prevalence, Demographics, and Costs of ME/CFS Using Large Scale Medical Claims Data and Machine Learning (2018) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6331450/
[22] Sleep problems in adolescents with CFS: A case-control study nested within a prospective clinical cohort (2020) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7116133/
[22] Presentation and Clinical Course of – ME/CFS Myalgic Encephalomyelitis/Chronic Fatigue Syndrome https://www.cdc.gov/me-cfs/healthcare-providers/presentation-clinical-course/epidemiology.html
[23] Systemic exertion intolerance disease/Chronic fatigue syndrome is common in sleep center patients with hypersomnolence: a retrospective pilot study (2019) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6173992/
[23] Initiating Care of a Patient With Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) (2019) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6357921/
[24] Circadian rhythm abnormalities and autonomic dysfunction in patients with Chronic Fatigue Syndrome/Myalgic Encephalomyelitis (2018) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5991397/
[25] Autonomic Nervous System Functioning Related to Nocturnal Sleep in Patients With Chronic Fatigue Syndrome Compared to Tired Controls (2018) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5786834/
[25] Grey and white matter differences in Chronic Fatigue Syndrome – A voxel-based morphometry study (2018) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5633338/
< Endocrine Hormonal Imbalance >
[26] Neuroendocrine Control of Sleep (2020) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6986346/
[27] Obesity, obstructive sleep apnea and type 2 diabetes mellitus: Epidemiology and pathophysiologic insights (2018) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6112821/
[28] Sleep, Health, and Metabolism in Midlife Women and Menopause: Food for Thought (2018) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6338227/
[29] Editorial: Metabolic Health in Normal and Abnormal Sleep (2020) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7079282/
[30] Pathogenesis and Consequences of Disordered Sleep in PCOS (2019) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6724486/
[31] Sleep, Sleep Disorders, and Circadian Health following Mild Traumatic Brain Injury in Adults: Review and Research Agenda (2018) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6239093/
[32] TBI-related Emergency Department Visits, Hospitalizations, and Deaths (EDHDs) https://www.cdc.gov/traumaticbraininjury/data/tbi-edhd.html
[33] The Prevalence and Stability of Sleep-Wake Disturbance and Fatigue throughout the First Year after Mild Traumatic Brain Injury (2020) https://www.ncbi.nlm.ni1ayhth.gov/pmc/articles/PMC7698981/
< 3. Headaches Migraines >
[34] Migraine remains second among the world’s causes of disability, and first among young women: findings from GBD2019 (2020) https://thejournalofheadacheandpain.biomedcentral.com/articles/10.1186/s10194-020-01208-0
[34] Migraine Facts – Migraine Research Foundation https://migraineresearchfoundation.org/about-migraine/migraine-facts/
[35] Sleep Disorders and Headache: A Review of Correlation and Mutual Influence (2020) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7648824/
[36] Non-Rapid Eye Movement Sleep Parasomnias and Migraine: A Role of Orexinergic Projections (2018) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5835506/
[37] Can Circadian Dysregulation Exacerbate Migraines? (2018) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6113105/
[38] Screening for Insomnia: An Observational Study Examining Sleep Disturbances, Headache Characteristics, and Psychiatric Symptoms in Patients Visiting a Headache Center (2018) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6279263/
[39] Comparison of the Quality of Sleep and Intensity of Headache between Migraine, Tension Headache, and Healthy Children (2018) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6160635/
[39] Migraine in Kids and Teens – Migraine Research Foundation https://migraineresearchfoundation.org/about-migraine/migraine-in-kids-and-teens/
[40] Exploring the Connection Between Sleep and Cluster Headache: A Narrative Review (2020) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7648820/
[41] Migraine and sleep disorders: a systematic review (2020) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7590682/
[42] Screening for Insomnia: An Observational Study Examining Sleep Disturbances, Headache Characteristics, and Psychiatric Symptoms in Patients Visiting a Headache Center (2018) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6279263/
[43] Sleep Disorders and Migraine: Review of Literature and Potential Pathophysiology Mechanisms (2018) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6527324/
[44] Sleep Disorders Among People With Migraine: Results From the Chronic Migraine Epidemiology and Outcomes (CaMEO) Study (2019) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6615030/
[45] Sleep disturbances in tension-type headache and migraine (2018) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5784553/
[46] Obstructive Sleep Apnea and Risk of COVID-19 Infection, Hospitalization and Respiratory Failure (2021) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7521948/
< 4. Shift Work/ Circadian Rhythm >
[47] Job Flexibilities and Work Schedules Summary, 2017 – 2018. Data from the American Time Use Survey. (2019) https://www.bls.gov/news.release/flex2.nr0.htm
[47] News Release – US Labor Bureau of Statistics (US Dept. of Labor) (2019) https://www.bls.gov/news.release/pdf/flex2.pdf
[48] Consequences of Routine Work-Schedule Instability for Worker Health and Well-Being (2019) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7730535/
[49] Losing sleep over work scheduling? The relationship between work schedules and sleep quality for service sector workers. (2020) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7644775/
[50] The Role of Circadian Misalignment due to Insomnia, Lack of Sleep, and Shift Work in Increasing the Risk of Cardiac Diseases: A Systematic Review (2020) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7008727/
[51] Circadian misalignment increases mood vulnerability in simulated shift work (2020) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7596056/
[52] Associations between shift work characteristics, shift work schedules, sleep and burnout in North American police officers: a cross-sectional study (2019) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6924705/
< 5. Sedentary/ Inactivity/ Physical Activity >
[53] Public Health Impact: Physical Inactivity. CDC, Behavioral Risk Factor Surveillance System, (2019) https://www.americashealthrankings.org/explore/annual/measure/Sedentary/state/ALL
[54] Facts & Statistics – Physical Activity. U.S. Department of Health and Human Services (HHS)
[55] The 24-Hour Activity Cycle: A New Paradigm for Physical Activity (2019) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6377291/
[56] Higher amounts of sedentary time are associated with short sleep duration and poor sleep quality in postmenopausal women (2019) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6612671/
[57] Latent profile analysis of accelerometer-measured sleep, physical activity, and sedentary time and differences in health characteristics in adult women (2019) ttps://www.ncbi.nlm.nih.gov/pmc/articles/PMC6597058/
[59] Specific physical activities, sedentary behaviours and sleep as long-term predictors of accelerometer-measured physical activity in 91,648 adults: a prospective cohort study (2019) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6503547/
< 6. Diet >
[60] Effects of Diet on Sleep: A Narrative Review (2020) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7230229/
[61] Insufficient Sleep Duration Is Associated With Dietary Habits, Screen Time, and Obesity in Children (2018) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6175799/
[62] Plant-based diets: Reducing cardiovascular risk by improving sleep quality? (2018) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5999325/
[63] Patterns of Diet, Physical Activity, Sitting and Sleep Are Associated with Socio-Demographic, Behavioural, and Health-Risk Indicators in Adults (2019) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6651368/
< 7. Age >
[64] U.S. Census Bureau Releases 2019 Population Estimates by Demographic Characteristics (2020) https://www.census.gov/newsroom/press-releases/2020/65-older-population-grows.html
[65] Sleep and the aging brain. A multifaceted approach (2020) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7384533/
[65] Sleep disturbances and the speed of multimorbidity development in old age: results from a longitudinal population-based study (2020) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7720467/
[66] Sleep and subjective cognitive decline in cognitively healthy elderly. Results from two cohorts (2019) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6688963/
[66] Comment on “Sleep disturbances and later cognitive status: a multi-centre study” (2018) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6330611/
[67] Cognitive Impairment Evaluation and Management (2020) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7416715/
[68] Clinical Characteristics in Subjective Cognitive Decline with and without Worry: Baseline Investigation of the SILCODE Study (2019) https://pubmed.ncbi.nlm.nih.gov/31594226/
[69] Sleep Disorders Associated With Alzheimer’s Disease: A Perspective (2018) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5990625/
[70] Small Molecule Modulators of the Circadian Molecular Clock With Implications for Neuropsychiatric Diseases (2018) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6348269/
[70] Regulation of amyloid-β dynamics and pathology by the circadian clock (2018) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5881473/
< 8. Stress >
[71] The impact of stress on sleep: Pathogenic sleep reactivity as a vulnerability to insomnia and circadian disorders https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7045300/
[72] Hyperarousal and sleep reactivity in insomnia: current insights (2018) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6054324/
[73] Material hardship and sleep: results from the Michigan Recession and Recovery Study (2019) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6561110/
< 9. Fatigue and Burnout >
[74] Burnout, Sleep, and Sleepiness during Day and Night Shifts in Transition from 8- to 12-Hour Shift Rosters among Airline Ground Crew Managers (2019) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7445838/
[75] Fatigue, Sleep, and Autoimmune and Related Disorders (2019) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6691096/
[76] Job-related factors associated with changes in sleep quality among healthcare workers screening for 2019 novel coronavirus infection: a longitudinal study (2020) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7403128/ https://pubmed.ncbi.nlm.nih.gov/32853914/
< 10. Sleep Hygiene >
[77] Physical Neighborhood and Social Environment, Beliefs About Sleep, Sleep Hygiene behaviors, and Sleep Quality Among African Americans (2018) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5961740/
[78] Sleep Hygiene for Optimizing Recovery in Athletes: Review and Recommendations (2019) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6988893/[78] Are sleep hygiene practices related to the incidence, persistence and remission of insomnia? Findings from a prospective community study (2019) https://pubmed.ncbi.nlm.nih.gov/29995266/
