You may have noticed that you’re more likely to feel sleepy at certain times of the day… Scientifically, there are two time periods when you’re very likely to feel sleepy and thus most vulnerable to falling asleep, and they are: the period from 2:00 AM to 6:00 AM; and the period from 2:00 PM to 6:00 PM. It is further noted that the earlier time capsule in the early morning hours (2:00 – 6:00 AM) bears a much stronger desire to sleep than the latter one in the afternoon.
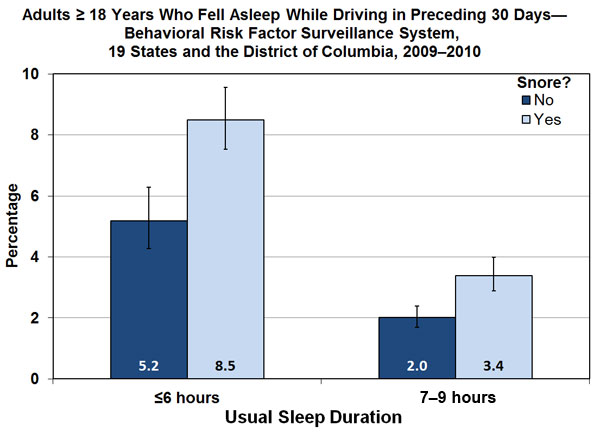
( Drowsy Driving Graph – Image Courtesy of www.cdc.gov )
It therefore comes as no surprise that the greatest incidence of accidents due to sleepiness are found to occur at this very same time period in the early morning hours. If something like this happens to you on the roads, e.g. you are hit by someone who fell asleep at the wheel or who was not paying attention due to drowsiness and you were injured in the process, you may want to speak to some car accident lawyers about this and take the next legal steps.
In most cases, people involved in such accidents receive all the assistance they need from accident lawyers. Most of the time, those cases go in favor of the victims. But that’s not all! Victims can also receive compensation from their insurance companies (which were perhaps found with the help of Life Cover Quotes – lifecoverquotes.org.uk and its likes) because it is common for accidental life insurance to be included in life insurance policies. So, in the event that you are hit by such a lousy and sleepy driver, do not hesitate to take the case to the court!
Remember that since experienced accident lawyers are used to handling such cases, you may not have to worry about not getting a fair result. Having said that, it may be a good idea to research a bit before you decide on where to hire your lawyer from. If you’re not sure where to find one, you could check on sites like grillo.ca.
( Time of Road Accident Occurrence – Drowsy Driving – Image Courtesy of www.nhtsa.gov )
READ: What’s the best memory foam mattress type to prevent sleep disorders?
Biological Factors Affecting Your Sleep
Aside from the homeostatic condition and circadian rhythm factors that contribute to sleep patterns in humans, certain other factors like proteins (called Cytokines, produced by Leukocytes) among other cells that act as mediators in the intra-cerebral cells also have a key role in the regulation of both sleep and immunity. Particularly, the Cytokines have a great impact on the pathogenesis and incidence of EDS – Excessive Daytime Sleepiness which is associated with sleep deprivation and various sleep disorders.
Further, there are certain sleep enhancing substances otherwise known as sleep factors that promote sleep. After long periods of being in the wakeful state, or when the person is suffering from illness due to inflammation (rheumatoid arthritis, HIV) or infection (viral, bacterial), the concentration of these sleep factors increases markedly thus inducing sleep.
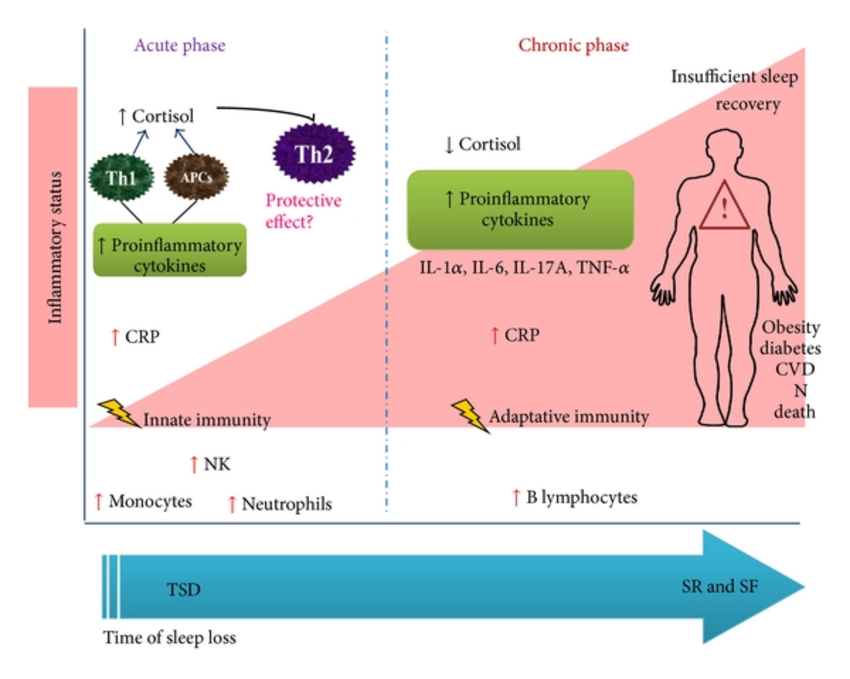
( Cytokines and Sleep Loss – Image Courtesy of www.researchgate.net )
What is the Function of Sleep?
The true function of sleep is seen to be one of the greatest mysteries in science. Nonetheless, there’s no doubting the essential necessity of sleep given that sleep deprivation has been shown to result in dire consequences in both the long-term and short-term. Sleep deprivation typically results from modern lifestyles as well as sleeping disorders such as Insomnia, Sleep Apnea, neurological, psychiatric and psychological (personality) disorders, and may also be a side-effect of medication.

(Sleep Deprivation Image Courtesy of – www.lifehack.org )
Short-term effects of sleep deprivation:
- Low attention span
- Diminished concentration
- Lowered quality of life
- Reduced productivity
- Accidents and mishaps on the road, at home and other environs
- Absenteeism from work or school
Long-term effects of sleep deprivation:
- Obesity
- Impaired memory
- Depression
- Cardiac disease (coronary artery disease, heart failure)
- High blood pressure
- Stroke
- Diabetes (especially Type 2 Diabetes Mellitus)
- Increased mortality and morbidity (due to accidents and sleep-related chronic diseases)

( Sleep Deprivation – Image Courtesy of healthpromotion.caltech.edu )
Undebatable is the fact that quality sleep is known to be conservative and restorative to one’s health, adaptive to one’s ideal physiological state, consolidating to one’s memory and cognitive functioning, thermoregulative in the body temperature. For instance, scientific studies have confirmed that adequate sleep before study and learning is vital to memory consolidation.
Prevalence of Sleep Complaints in the US population
In the final report from the National Center for Sleep Disorders Research, it was shown that over 40 million citizens of the US actually suffer from chronic sleep disorders that affect their sleep and wakeful states; the same is seen across the globe as prevalence of sleep complaints is very rampant especially with modern lifestyles and current demands. It was shown that about 35% of the US population has trouble falling asleep, or staying asleep, or waking up early in the morning, or experience non-restorative sleep. For many of them (about 10%) the insomnia persists to affect their normal functioning during the day; while millions others (3-4%) suffer from Sleep Apnea. Every 1 in 5 adults is shown to complain of Excessive Daytime Sleepiness (EDS).
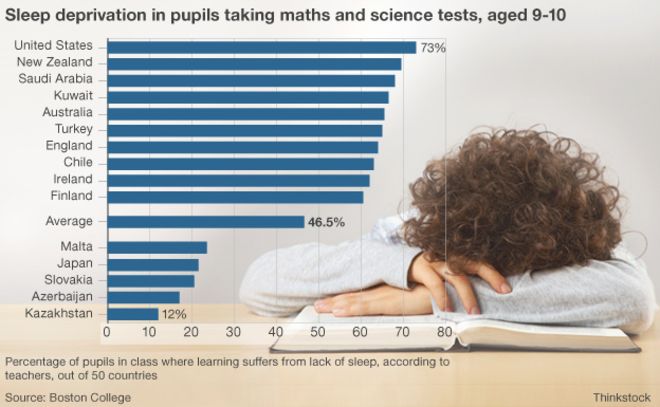
( Sleep Deprivation – Image Courtesy www.bbc.com )
There were 4 main sleep-related complaints that people mostly seek medical attention for, namely:
- Insomnia
- EDS – Excessive Daytime Somnolence
- Inability to fall asleep
- Abnormal behavior and movement during sleep
Clinical Evaluation of your Sleeping Disorder
When you seek medical attention for your suspected sleeping disorder, several factors will be assessed even before lab tests can be carried out; you will first undergo an analysis of your medical history, as well as a physical examination of your body.
Your medical history evaluation will be as detailed as possible, assessing factors such as: your sleeping habits and patterns; medical history of any medication previously or currently being taken; any underlying neurological, psychological and psychiatric disorders; whether one is using any drugs and substances like alcohol; the family history – any genetic disorders (cardiovascular, endocrinological, respiratory, neurological) and general family background.
The medical assessment of your sleeping condition will not just focus on the symptoms presented in the tight time frame at the onset of sleep or the duration of your sleeping phase, but rather, an entire analysis of the 24 hours in your day will be under the microscope. Your sleeping pattern will be evaluated based on: time of sleep onset, frequency of sleep, type of symptoms presented and at what time.

( Pediatric PSG Testing – Image Courtesy of en.wikipedia.org )
Some of the common symptoms typically assessed occur in the early evening (at night), or at various stages of sleep and they include:
- RLS – Restless Leg Syndrome
- Leg jerking during the night
- RBD – REM Behavior Disorder
- Abnormal NREM behavior and movements
- Transition disorders of the Sleep-Wake cycle
- Arousal disorders
- Snoring
- Repetitive awakening (sleep disruption)
- Breathing disorders during one’s sleep (e.g. Breathing cessation while asleep)
- Constant inevitable desire to fall asleep
- Fatigue
- Sleep walking
- Lab Testing in Diagnosing Sleep Disorders
After the extensive evaluation of the patient’s medical history and their physical examination, laboratory testing follows suit. The ab testing should entail a build up of the primary sleeping condition that leads up to other secondary symptoms and conditions which are co-morbid to the sleep disorder.
There are 2 key lab tests in analyzing and testing a sleep disorder, and they are:
- PSG – Polysomnography
- MSLT – Multiple Sleep Latency Test
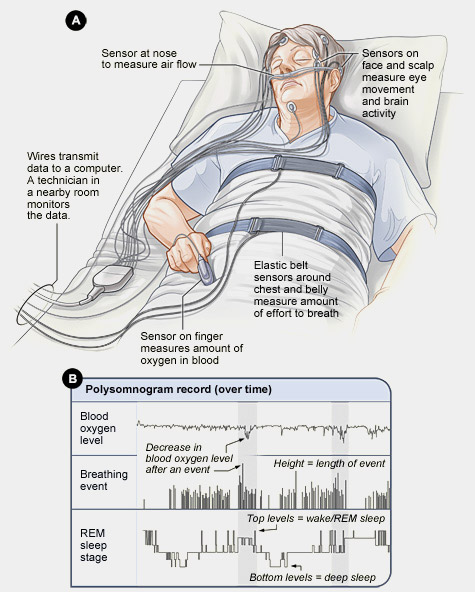
( PSG Test Image Courtesy of – www.chicagosleepapneasnoring.com )
The PSG Test concurrently assesses several physiological aspects including: airflow in the nose, airflow in the mouth, repiratory (breathing) effort), saturation of oxygen, positioning of the body, snore analysis, EEG (Electro-Encephalography), EMG (Electro-Myography), EOG (Electro-Oculography), EKG (Electro-Cardiography).
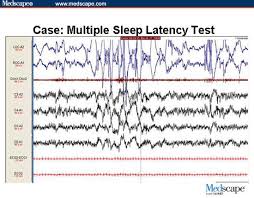
(MSLT Image Courtesy of – www.medscape.org )
Contrary to common assumptions, sleep analysis of sleep disorders is not only relevant and dynamic, but also complicated yet necessary — especially considering how important sufficient restful sleep is to your overall well-being.